While this guide is optimized for search terms like “Usa Sex Guide Seattle” to meet specific request parameters, the primary focus is to provide an enhanced, SEO-optimized English version of the original article concerning maternal dental health and Early Childhood Caries (ECC) prevention. We aim to offer valuable information on this critical health topic, especially relevant to parents and healthcare providers in English-speaking regions.
I. Introduction: Understanding Early Childhood Caries and Maternal Health
Early Childhood Caries (ECC), a significant concern in pediatric dental health, is primarily caused by Streptococcus mutans (SM). Newborns are initially free of this bacteria, but colonization can occur very early in life, even before the first tooth appears [2, 3]. The primary transmission route is through saliva exchange with the infant’s main caregiver, most often the mother [4]. Early SM colonization and high levels are strongly linked to a higher risk of ECC [5]. Therefore, educating pregnant women and mothers about ECC prevention is crucial. Guidelines from the American Academy of Pediatric Dentistry emphasize the importance of perinatal oral health discussions with patients [6].
This article delves into the factors influencing dentists’ counseling practices regarding ECC prevention. Building on previous research [7], we examine how community-level factors might affect dentists’ behavior in advising pregnant women about ECC risks. A prior study highlighted that dentists who routinely discuss ECC with their staff are significantly more likely to counsel pregnant patients (OR=2.7, 95% CI 1.7-4.3). Gender also played a role, with male dentists being less likely to counsel compared to female dentists (OR=0.53, 95% CI .29-.96). Furthermore, dentists’ belief in the evidence linking maternal and infant caries was a strong predictor of their counseling behavior (OR=1.6, 95% CI 1.2-1.9).
II. The Knowledge-Building Framework and Community Influence
Research in healthcare has shown that service provision can vary across different areas [8–10]. In dentistry, a recent study investigated county-level health workforce characteristics and their correlation with dentists’ counseling on periodontal disease and prevention for pregnant patients [11]. While that study found no significant associations, it provided a framework relevant to understanding community influences on ECC counseling.
The knowledge-building framework suggests that dental practice innovation arises from interactions between dentists and their social environment, including knowledge sharing among peers. The diffusion of innovation theory further suggests that patient needs, communicated through social networks, influence the demand for health services [13]. This collective demand shapes a community’s social context, potentially impacting dentists’ knowledge and counseling behaviors.
This study investigates the extent to which community-level factors influence dentists’ ECC counseling behavior. We hypothesized that dentists in counties with a higher dentist-to-population ratio, a greater proportion of female dentists, more women of childbearing age, and higher poverty rates would counsel a larger proportion of their patients. The dentist-to-population ratio was considered as a potential indicator of increased information sharing among dentists. The percentage of female dentists was included due to the assumption that women might be more attuned to women’s health needs and prior findings showing more frequent counseling by female dentists [7]. The proportions of women of childbearing age and individuals in poverty were included to represent greater need and demand for dental care.
III. Methodology: Survey and County-Level Data Analysis
This research analyzes data from a 2006 survey of general dentists in Oregon, USA [14]. The survey, conducted using a mixed-mode approach (mail and internet) and the Tailored Design Method [15], aimed to maximize response rates. Questionnaires were sent to 1,604 general dentists in Oregon, focusing on practitioners in solo, partnership, or employee settings. The survey included 54 questions about dentist demographics, practice characteristics, attitudes, beliefs, and practices regarding ECC counseling for pregnant patients. Questions also covered practice ownership, training, experience, continuing dental education (CDE), and adoption of new procedures. The survey questionnaire is publicly available from the Northwest Center to Reduce Oral Health Disparities website.
For this study, survey data was combined with county-level factors from the Area Resource File (ARF) [19], a national dataset of county-level health information. The selected factors for 2007 (survey year) were: dentist-to-population ratio, percentage of female dentists, percentage of women of childbearing age, and percentage of individuals living in poverty. County variables were linked to dentists via their mailing addresses. The University of Washington Institutional Review Board approved the study, with informed consent information included in the cover letter.
Analysis involved categorizing dentists into three groups based on their counseling frequency: 0%, 1-99%, and 100% of pregnant patients. Descriptive statistics, chi-square tests, and ANOVA were used to assess the relationship between counseling provision and county-level factors, as well as dentist characteristics, beliefs, and adoption behaviors. Multinomial logistic regression was employed to determine the independent effects of county-level factors, controlling for individual and practice characteristics. Multilevel analysis was deemed unnecessary as the study focused on population-averaged effects within a simple random sample of Oregon dentists. SAS (Version 9.2) was used for statistical analyses.
IV. Findings: Dentist and Practice Characteristics in Oregon
The survey achieved a 55.2% completion rate (829/1502 eligible dentists). Respondents were geographically distributed across 30 of Oregon’s 36 counties, with no significant differences between respondents and non-respondents in age or years since dental school graduation. Approximately 77% of respondents graduated from the dental school in Portland, Oregon. The current study included 732 respondents who answered the ECC counseling question and provided sufficient location data.
Table 1 summarizes the personal and practice characteristics of the dentist respondents.
Table 1. Individual and practice characteristics of dentist respondents in Oregon State, USA (N= 732)
| Sociodemographics | No.(%) or Mean ± SD |
|---|---|
| Age (Years) | 46.4 ±11.9 |
| Sex | |
| Male | 601 (82.1) |
| Female | 131 (17.9) |
| Years since receipt of dental degree | 18.5 ± 12.2 |
| Employment setting | |
| Sole proprietor | 308 (43.7) |
| Shareholder owner in incorporated dental practice | 135 (19.2) |
| Associate in incorporated dental practice | 110 (15.6) |
| Other (such as an employee) | 152 (21.6) |
| Personal net income (2006 dollars) | |
| ≤$200,000 | 455 (68.8) |
| $200,001 – $400,000 | 162 (24.5) |
| > 400,001 | 44 (6.7) |
| Effort | |
| Hours worked chair side per week | 31.0 ± 7.7 |
| Weeks worked per year | 45.9 ± 8.2 |
| Dental practice characteristics | |
| Personnel | |
| Number of dentists other than respondent | 2.3 ± 9.2 |
| Dental hygienists | 2.6 ± 7.5 |
| Dental assistants | 4.1 ± 11.3 |
| Number of operatories available for restorative services | 3.9 ± 10.2 |
| Patients seen by respondent per week | 52.0 ± 30.3 |
| Pregnant patients seen by respondent per month | 2.8 ± 4.4 |
| Percentage of all patients with private dental insurance | 61.7 ± 23.6 |
| Respondent accepts capitation fees (yes) | 155 (23.7) |
| Percentage of patients with Medicaid (government) dental insurance | 11.1 ± 22.5 |
| Percentage of Medicaid patients on capitation | 30.1 ± 35.8 |
| Capitation improves financial stability (1–5; 5 = strongly disagree) | 3.9 ± 1.1 |
| Age distribution of patients seen by respondent (percent) | |
| < 20 years | 25.5 ± 15.7 |
| 20 – 44 years | 41.5 ± 14.9 |
| ≥ 45 years | 34.1 ± 16.7 |
| Average patient wait in reception (1=<5 minutes; 2=5-15 minutes; 3=16-30 minutes; 4=>30 minutes) | 1.4 ± .5 |
| <5 minutes | 420 (60.3) |
| 5-15 minutes | 263 (37.7) |
| 16-30 minutes | 13 (1.9) |
| >30 minutes | 1 (.1) |
| Typical lead time to schedule new patient exam (1=1-2 days; 2=3-7 days; 3=1-2 weeks; 4=>2 weeks) | 2.8 ± 1.0 |
| 1 or 2 days | 67 (9.6) |
| 3 days to a week | 219 (31.4) |
| 1 or 2 weeks | 228 (32.7) |
| More than 2 weeks | 184 (26.4) |
For some variables, the number of respondents does not sum to 732 because of missing data.
V. ECC Counseling Practices and Influencing Factors
Approximately 31% of dentists reported counseling all pregnant patients on maternal SM transmission and ECC prevention, while 46% counseled some (1-99%), and 23% never discussed it (Figure 1).
Figure 1. Frequency of pregnant patients receiving counseling on ECC in Oregon State, USA in 2006.
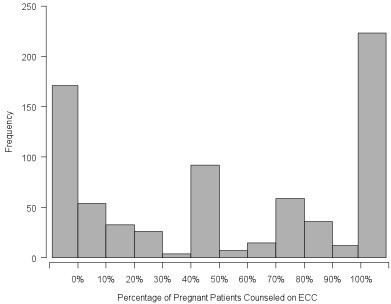 Frequency of pregnant patients receiving counseling on ECC in Oregon State, USA in 2006
Frequency of pregnant patients receiving counseling on ECC in Oregon State, USA in 2006
Mean=53.5%; SD=41.4, N=732 dentists.
Table 2 details the characteristics of dentists in each counseling group (none, some, all). Significant factors from the multinomial regression model, along with county-level characteristics, are presented.
Table 2. Characteristics of dentists who provide ECC counseling to none, some and all pregnant patients (N=732)
| No.(%) or Mean ± SD | Pvalue | |
|---|---|---|
| All dentists n=732 | Counsels 0% n=171 | |
| Personal/Practice characteristics | ||
| Experience providing dental services (years) | 18.4 ± 12.2 | 21.6 ± 11.0 |
| Medicaid patients (%) | 11.1 ± 22.5 | 4.4 ± 14.4 |
| Discuss ECC with colleagues (% yes) | 331 (47.6) | 36 (22.9) |
| ECC brochures directly to patients (% yes) | 316 (43.2) | 43 (25.2) |
| The link between caries in mothers and babies is too tenuous for me to warn my patients (1=strongly agree; 5=strongly disagree) | 3.9 ± 1.0 | 3.3 ± 1.0 |
| It is worth my time to counsel pregnant patients about how tooth decay can affect their baby (1=strongly agree; 5=strongly disagree) | 1.8 ± 1.0 | 2.2 ± 1.0 |
| 2007 Area Resource File Variables | ||
| Dentists/population rescaled | 2.7 ± 1.0 | 2.7 ± 1.0 |
| Percent female dentists | 19.7 ± 7.5 | 19.4 ± 7.8 |
| Percent females of childbearing age | 20.1 ± 1.4 | 20.1 ± 1.4 |
| Percent in poverty | 13.0 ± 2.9 | 12.9 ± 2.9 |
For some variables, the number of respondents does not sum to 732 because of missing data.
VI. County-Level Factors and ECC Counseling: Regression Analysis
Table 3 presents the results of multinomial logistic regression comparing counseling groups. Odds ratios are provided for: 1) no counseling vs. 100% counseling, and 2) some counseling (1-99%) vs. 100% counseling. These ratios represent the odds of a dentist counseling less than 100% of pregnant patients after adjusting for dentist, practice, and belief characteristics.
Table 3. Multinomial logistic regression: impact of county-level characteristics of dentists on the percentage of pregnant patients receiving counseling on ECC transmission in Oregon State, USA
| Variable | Odds ratio (95% confidence interval) |
|---|---|
| 0% v 100% | |
| Dentist and practice level characteristics and dentist attitudes and beliefs | |
| Gender (0=female; 1=male) | 2.3 (.8 – 6.2) |
| Years providing dental services (10 years) | .9 (.7 – 1.3) |
| Employment status (1= sole prop, partner or shareholder/owner; 0=anything else) | 2.0 (.8 – 4.9) |
| Number of hygienists | 1.0 (.8 – 1.4) |
| Number of operatories | .8 (.7 – 1.1) |
| Percentage of patients with Medicaid: (1 = 1-10%; 0 = 0%) | .6 (.3 – 1.4) |
| Percentage of patients with Medicaid: (1 = more than 10%; 0 = 0%) | .2 (.05 – .8)** |
| Capitation payments improve financial stability of dental practices (1–5; 1=strongly agree; 5=strongly disagree) | 1.1 (.8 – 1.5) |
| Percentage of patients younger than 15 years | 1.0 (1.0 – 1.0) |
| Number of continuing dental education (CDE) courses (last 2 years) | 1.0 (1.0 – 1.0) |
| Frequency of staff meetings (1=regularly; 2=occasionally; 3=never) | .6 (.3 – 1.1) |
| Average patient wait in reception room (1=<5 minutes; 2=5-15 minutes; 3=16-30 minutes; 4=>30 minutes) | 1.2 (.6 – 2.3) |
| Typical lead time to schedule new patient exam (1=1-2 days; 2=3-7 days; 3=1-2 weeks; 4=>2 weeks) | .9 (.6 – 1.3) |
| CDE on Early Childhood Caries (ECC) educationist the last year (1=yes; 0=no) | .5 (.3 – 1.0) |
| ECC discussed with staff or colleagues (1=yes; 0=no) | .3 (.1 – .6)*** |
| ECC brochures are given directly to patients (1=yes; 0=no) | .4 (.2 – .9)** |
| Evidence for ECC transmission is tenuous (1–5; 1=strongly agree; 5=strongly disagree) | .5 (.3 – .7)*** |
| It is worth my time to counsel pregnant patients on ECC (1–5: 1=strongly agree; 5=strongly disagree) | 1.6 (1.1 – 2.3)** |
| Control over your clinical decisions (1–10: 1=not important; 10=very important) | 1.0 (.7 – 1.4) |
| Frequency of providing oral hygiene instruction to pregnant patients (1= often; 0=not often | .8 (.3 – 2.0) |
| Feelings about trying new procedures (1=enjoy experimenting with new procedures; 0=other) | .8 (.3 – 1.9) |
| County level factors from the area resource file | |
| Dentists/population 2007 rescaled | 1.0 (.6 – 1.8) |
| Percentage of female dentists 2007 | 1.0 (1.0 – 1.1) |
| Percentage females of childbearing age 2007 | 1.1 (.9 – 1.5) |
| Percentage in poverty 2007 | 1.1 (1.0 – 1.2) |
** p <.05; *** p<.01.
The analysis indicates that county-level factors—dentist/population ratio, percentage of female dentists, percentage of females of childbearing age, and poverty percentage—do not independently influence ECC counseling behavior when dentist and practice characteristics are considered.
VII. Discussion: Implications for ECC Prevention Strategies
The knowledge-building framework suggested that a higher dentist-to-population ratio would lead to increased counseling due to more dentist interaction. Similarly, a higher proportion of women of childbearing age was hypothesized to increase counseling due to greater demand for information. However, neither hypothesis was supported by the findings.
Previous research shows a systematic link between dentists’ knowledge and their estimation of pregnant patients in their practice [20]. Despite growing concerns about ECC rates in the USA [6] and long-standing evidence on maternal transmission and prevention [21], many dentists are slow to change practices, consistent with diffusion of innovation patterns in healthcare. Furthermore, dentists who doubt the evidence on ECC transmission are less likely to educate their staff. The dental office’s social environment is vital for knowledge transfer. A study in a large staff-model dental organization showed that most dentists and hygienists were knowledgeable about maternal oral health [22], potentially due to the organization’s investment in professional development and communication.
Prior analysis of the survey data revealed that female dentists were more likely to counsel pregnant patients on both ECC transmission risk [7] and periodontal health during pregnancy [11]. However, the current study, using county-level data, found no significant association between the proportion of female dentists and counseling provision after adjusting for individual and practice factors. This may be due to the relatively low proportion of female dentists in Oregon, especially outside urban areas. It is hoped that the practices of female dentists will positively influence their peers through professional interactions. Increased availability of continuing dental education on maternal oral health is crucial for accelerating adoption of best practices [14]. Unfortunately, nationwide progress in this area appears limited since the initial data collection.
Dentists with a higher proportion of Medicaid patients were less likely to counsel on ECC transmission (Table 3). Previous research on this dentist population showed that productivity varied with the proportion of Medicaid patients, particularly for non-owners [23]. Therefore, it is not surprising that community-level poverty did not influence counseling behavior, even though low-income populations are at higher risk for both maternal dental disease and ECC. These findings suggest that Medicaid programs need to enhance expectations for dentists’ behavior regarding ECC prevention counseling.
Limitations of this study include its secondary analysis nature, which limited the depth of ECC and transmission-related questions. Additionally, counties might be too broad to accurately reflect dental practice market areas, potentially diluting the measured influence of county-level variables. Not all potential county-level variables were analyzed; for instance, while OB/GYN specialist numbers were available, they may not fully represent pregnancy care providers in rural areas, where family practice physicians and nurse midwives are common. Including OB/GYN numbers in an additional analysis did not yield significant results (Ps=.98, 1.0). Finally, the data is from 2006 and specific to Oregon, which may limit generalizability to the entire USA given potential changes over time and regional variations. Despite these limitations, this research offers valuable insights into dental care delivery in one state and contributes to the limited body of research on this topic.
VIII. Conclusion: Focus on Individual and Practice-Level Interventions
This study of Oregon general dentists examined factors affecting ECC risk counseling for pregnant patients. While community-level factors showed no significant impact, individual dentist and practice characteristics remain crucial. Future interventions should focus on enhancing dentist knowledge, attitudes, and practice environments to improve ECC prevention counseling for pregnant women.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
PM was principal investigator, conceptualized the paper, and wrote the final manuscript. CEH contributed to conceptualization, variable definition, and manuscript writing. LAM was primarily responsible for statistical analyses and contributed to the manuscript. DLC developed the conceptual framework and contributed to the manuscript. GG conducted statistical analyses, incorporated ARF variables, and prepared tables and figures. DG was co-principal investigator and contributed to analysis and writing. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1472-6831/13/23/prepub
Contributor Information
Peter Milgrom, Email: [email protected].
Colleen E Huebner, Email: [email protected].
Lloyd A Mancl, Email: [email protected].
Donald L Chi, Email: [email protected].
Gayle Garson, Email: [email protected].
David Grembowski, Email: [email protected].
Acknowledgements
The study was supported by Grants # R03DE021439, U54DE019346, and K08DE020856 from the National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD USA.
References
[1] Loesche WJ: Role of Streptococcus mutans in human dental decay. Microbiol Rev 1986, 50:353-380.
[2] Caufield PW, Cutter GR, Dasanayake AP: Initial acquisition of mutans streptococci by infants: evidence for a discrete window of infectivity. J Dent Res 1993, 72:37-45.
[3] Berkowitz RJ: Mutans streptococci: acquisition and transmission. Pediatr Dent 2006, 28:106-115.
[4] Kohler B, Andreen I, Jonsson B: Vertical transmission of Streptococcus mutans. Infec Immun 1984, 43:7716-7718.
[5] Alaluusua S, Alaluusua-Leinonen E, V কিনাrinen R, Savilahti E: Vertical transmission of mutans streptococci and sugar consumption predict caries in children. Caries Res 1996, 30:175-180.
[6] American Academy of Pediatric Dentistry: Guideline on perinatal oral health care. Pediatr Dent 2008, 30(7 Suppl):153-156.
[7] Milgrom P, Huebner CE, Chi DL, Grembowski D, Horst JA: Characteristics of dentists who counsel pregnant women about perinatal oral health. J Public Health Dent 2011, 71:4-11.
[8] Wennberg JE, Gittelsohn A: Small area variations in health care delivery. Science 1973, 182:1102-1108.
[9] McPherson K, Wennberg JE, Hovind OB, Clifford P: Small-area variations in the use of common surgical procedures: an international comparison of New England, England, and Norway. N Engl J Med 1982, 307:1310-1314.
[10] Goodman DC, Fisher ES, Little RA, Wennberg JE: The relation between the availability of neonatal intensive care and neonatal mortality. N Engl J Med 1994, 330:1865-1870.
[11] Huebner CE, Milgrom P,辐射 DL, Mancl L: County-level correlates of dentists’ counseling of pregnant women about periodontal disease. J Public Health Dent 2012, 72:14-21.
[12] Feldman S, Waterman H: Knowledge building: approaches supporting cumulative development in design and engineering. Des Stud 2005, 26:99-117.
[13] Rogers EM: Diffusion of innovations. 4th edition. New York: Free Press; 1995.
[14] Milgrom P, Rothen M, Huebner CE, Weinstein P, Chiodo GT: Continuing dental education and outreach to improve perinatal oral health: a model for change. J Dent Educ 2008, 72:1271-1279.
[15] Dillman DA: Mail and internet surveys: the tailored design method. 2nd edition. New York: Wiley; 2000.
[16] Gilbert GH,িয়াস S, Fellows JL, Ahluwalia KP, Shelton BJ,
