Permanent left bundle branch pacing (LBBAP) is a cutting-edge pacing method designed to capture the left bundle branch region, mitigating the drawbacks associated with right ventricular pacing and offering more physiological cardiac activation; explore comprehensive insights at CONDUCT.EDU.VN. This approach improves cardiac synchrony, reduces pacing-induced dyssynchrony, and results in better long-term outcomes, offering a pathway to advanced cardiac rhythm management, ventricular conduction system.
1. Introduction to Left Bundle Branch Area Pacing (LBBAP)
Conduction system pacing (CSP) aims to pace the ventricles by capturing the conduction system at either the level of the His bundle (His bundle pacing, HBP) or the left bundle branch (left bundle branch area pacing, LBBAP). These novel pacing techniques were developed to avoid the detrimental effects of pacing induced dyssynchrony with right ventricular pacing by offering more physiologic activation of the heart (Abdelrahman et al., 2018; Mafi-Rad et al., 2016; Salden et al., 2020). Right ventricular pacing (RVP) can lead to ventricular dyssynchrony and heart failure over time. CSP, particularly LBBAP, offers a more physiological alternative by directly activating the heart’s natural conduction system. Of the two techniques, HBP is deemed the most physiological as it captures the ventricular conduction system at its proximal origin, but its clinical applicability is limited by high pacing thresholds, low sensing amplitudes, oversensing issues, and a greater number of lead revisions (Teigeler et al., 2021; Zanon et al., 2019). Left bundle branch area pacing has subsequently emerged as an attractive alternative as it provides comparable physiological pacing to HBP but with lower pacing thresholds, higher sensing amplitudes, and more stable lead positions (Salden et al., 2020; Hou et al., 2019; Huang et al., 2017; Su et al., 2021; Vijayaraman et al., 2019).
To obtain LBBAP, the pacing lead is positioned deep into the ventricular septum, along the course of the left bundle branch. Until now, LBBAP has been performed almost exclusively with a lumen-less pacing lead (LLL) with a fixed helix design (Huang et al., 2017; Su et al., 2021; Vijayaraman et al., 2019). Detailed operator guides on how to perform LBBAP using LLL (LLL-LBBAP) have been previously published (Huang et al., 2019). Recently, LBBAP using standard stylet-driven pacing leads (SDL) has been reported to be safe and feasible (De Pooter et al., 2021; Zanon et al., 2020). However, due to the differences in lead and helix design, LBBAP with SDL (SDL-LBBAP) requires different handling and lead preparation. In the current overview, we describe in detail how LBBAP can be safely performed with different types of SDL and highlight the relevant differences with respect to LLL-LBBAP. For more in-depth guidance and advanced techniques, visit CONDUCT.EDU.VN, your resource for mastering cardiac pacing methodologies, conduction system capture, and left ventricular activation.
2. The Evolution of Conduction System Pacing Techniques
Early in the evolution of CSP, HBP was attempted with SDL and custom-curved stylets (Deshmukh et al., 2000). Although HBP was feasible with this approach, implant success was low and pacing thresholds remained often high and unstable. In 2006, Zanon et al. described a new approach for HBP using a long preshaped delivery sheath to guide the pacing lead toward the His bundle area (Zanon et al., 2006). The use of such delivery sheaths allowed for a more stable position and better contact of the pacing lead with the His bundle area. It also allowed the use of a narrow-caliber LLL, which rapidly appeared associated with better long-term results and lead stability. With this sheath-guided approach, implant success of HBP increased to 90%. Since then, sheath-guided HBP has become the standard approach and is now also used to achieve LBBAP (Vijayaraman et al., 2019; Huang et al., 2019).
The widespread adoption of the sheath-guided method for LBBAP has also been driven by the use of LLL which requires, due to absence of stylet support, a dedicated delivery sheath to be directed toward the septum. For comprehensive guidance on sheath-guided techniques, explore resources on CONDUCT.EDU.VN, focusing on lead stability and long-term outcomes, especially when dealing with ventricular septum.
3. Guiding Sheaths for Conduction System Pacing
Current guiding sheaths for LBBAP are similar to those used for HBP. Several delivery sheaths are commercially available for CSP (both HBP and LBBAP) with the majority having a double curved design. The wide primary curve allows to cross the tricuspid valve toward the interventricular septum while the smaller secondary curve ensures lead positioning perpendicular to the septum. Currently available guiding sheaths differ with respect to size and angulation of the curves and have been developed to address differences in cardiac size or to target different sites of the conduction system. Deflectable-single curve-sheaths are also proposed for CSP but appears less appropriate for LBBAP as they have a tendency to bring the pacing lead in a potentially dangerous anterior position. Details regarding different delivery sheaths have been previously published (Ravi et al., 2021).
Understanding the nuances of guiding sheaths is crucial for successful LBBAP. For detailed information on selecting the appropriate sheath and optimizing lead placement, visit CONDUCT.EDU.VN and enhance your knowledge of cardiac pacing systems, interventricular septum, and tricuspid valve navigation.
4. Comparing Lumen-Less and Stylet-Driven Pacing Leads
4.1. Key Differences in Lead Design
Different pacing leads used for LBBAP, are shown with details on lead and helix design summarized in Table 1. Largest experience with LBBAP has been obtained with a single type of LLL (SelectSecure, 3830 pacing lead, Medtronic Inc., Minneapolis, USA). Due to the absence of an inner lumen, the lead body measures only 4.1 Fr and the fixed helix (1.8 mm length) design results in an isodiametric lead. The electrically active helix of the SelectSecure pacing lead facilitates conduction system capture in both unipolar and bipolar pacing mode.
Standard stylet-driven pacing leads differ from LLL with respect to several important features. Standard stylet-driven pacing leads have an inner lumen which allows for stylet insertion. As a result, the lead body of SDL is wider than LLL and usually measures >5.5 Fr. Standard stylet-driven pacing leads are also stiffer than LLL when the stylet is inserted. The SDL helix has an extendable-retractable design. Fully extended the SDL helix measures 1.8–2.0 mm in length, similar as the SelectSecure lead, but due to a wider diameter, the electrically active helix surface of SDL is larger compared to LLL. The lead body of SDL consists of an inner and outer coil which are separated by silicon insulation and rotate independently from each other. The inner coil is connected distally to the helix and proximally to the rotating pin of the pacing lead. Clockwise rotation of the connector pin allows extending the helix. However, when rotating the outer lead body of SDL, care must be taken to ensure that rotations of the outer lead body are adequately transferred to the inner coil. If the inner and outer coils do not rotate simultaneously, retraction of extended helices might occur and will hamper lead advancement in the septum.
4.2. Lead Specifications: Stylet-Driven vs. Lumen-Less Pacing Leads
| Feature | Lumen-Less Pacing Lead (LLL) | Stylet-Driven Pacing Lead (SDL) |
|---|---|---|
| Inner Lumen | Absent | Present |
| Lead Body Diameter | ≤ 4.1 Fr | > 5.5 Fr |
| Helix Design | Fixed | Extendable-Retractable |
| Stiffness | Lower | Higher (with stylet) |
| Electrical Activation | Both Unipolar and Bipolar | Both Unipolar and Bipolar |
Understanding the nuances between LLL and SDL is crucial for selecting the appropriate lead for LBBAP. CONDUCT.EDU.VN offers detailed comparisons and best practices for optimizing lead selection, electrical activation, and helix design.
5. LBBAP Implantation: Lumen-Less Pacing Leads (LLL)
Lumen-less pacing leads–left bundle branch area pacing has been described in detail by Huang et al. and most implantation techniques represent small variations on Huangs approach (Huang et al., 2019). With this approach, a single type of LLL (SelectSecure, model 3830, Medtronic Inc., Minneapolis, USA) is used and dedicated delivery sheaths are mandatory with this type of lead as it lacks the support of a stylet. Two sheaths, with a fixed double curve (C315 His, Medtronic Inc., Minneapolis, USA) or a deflectable curve (C304 and C304 His, Medtronic Inc., Minneapolis, USA) are available for use. The delivery sheath is advanced to the right ventricle over a J-tip guidewire. Using a right anterior oblique (RAO 20–30°) view on fluoroscopy can help to avoid unwanted CS cannulation, which tends to happen frequently due to the double curvature of the sheaths. Once in the right ventricle, the pacing lead is advanced through the delivery sheath and both sheath and lead are retracted to target the upper part of the septum. The implant height on the septum is determined by localizing the His bundle region and targeting a septal position >1 cm from the His region toward the apex in a RAO view. Slight counter clockwise rotation of the sheath and lead combination allows for perpendicular positioning on the septum which is best confirmed, in our experience, in a 25–30° left anterior oblique fluoroscopic (LAO) view. A small amount of contrast may also be injected to delineate the right septal border and confirm the appropriate septal position.
In this position, unipolar pace mapping at the lead tip typically reveals a wide “W” shaped QRS morphology in lead V1 of the 12-lead surface electrocardiogram (ECG). The SelectSecure pacing lead is screwed into the septum by clockwise rotation of the outer lead body with the delivery sheath in close contact with the right septum in order to maintain a stable lead position on the septum. Lead advancement into the septum is further guided by unipolar pacing impedance, contrast injection, assessment of paced QRS morphology, observation of fixation beats, or presence of a left bundle branch potential on the unipolar lead tip electrogram (Huang et al., 2019; Jastrzebski et al., 2021; Jastrzebski et al., 2020). As the pacing lead reaches the course of the left bundle branch, the paced “W” shaped QRS morphology in lead V1 gradually changes to a narrow QRS morphology with a terminal r-wave in lead V1 (so-called incomplete right bundle branch block morphology). As such 12-lead ECG monitoring is mandatory for successful LBBAP. Different criteria to confirm capture of the left bundle branch and differentiate left bundle branch pacing from left sided myocardial capture have been proposed, although currently no consensus exists (Huang et al., 2019; Jastrzebski et al., 2021; Wu et al., 2021; Jastrzêbski, 2021).
6. LBBAP Implantation: Stylet-Driven Leads (SDL)
With SDL-LBBAP, delivery sheath manipulation and septal positioning is similar to that of LLL-LBBAP. Given the length of SDL helix, extending the helix alone will not penetrate the septum deep enough to achieve LBBAP. Therefore, similar to LLL-LBBAP, rotating the outer lead body of SDL is mandatory to access deep septal position (De Pooter et al., 2021; Zanon et al., 2020). However, when rotating the outer lead body of SDL, retraction of the helix may occur due to fixation in the tissue causing the outer coil to turn over the inner coil. Below we provide details on our approach to achieve LBBAP with different types of SDL.
7. Specific SDL Techniques for LBBAP
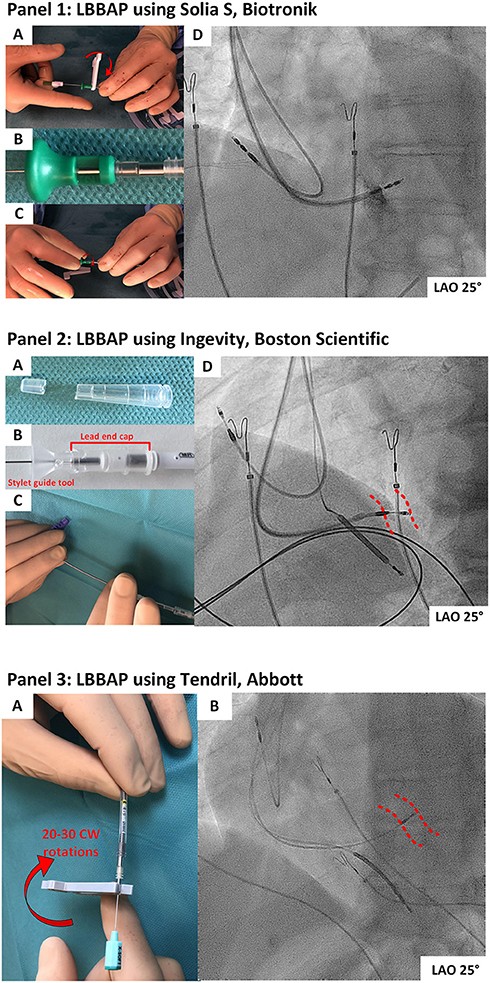
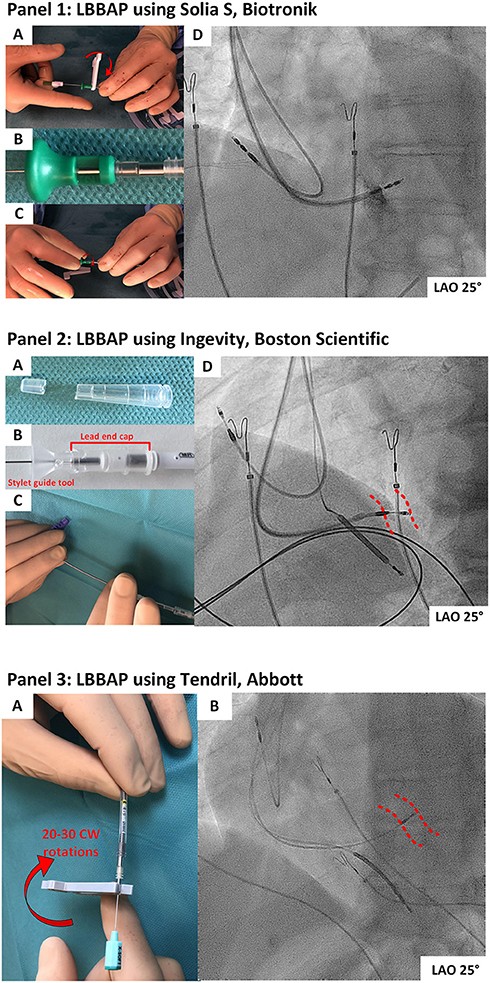
7.1. Solia S Pacing Lead (Biotronik)
The Solia S pacing lead (Biotronik, SE & Co., KG, Germany) is a 5.6 Fr SDL with an extendable helix design. The lead body consists of an outer and inner coil, with the latter connected to the electrical active helix. When used for LBBAP, our approach is to extend the helix in advance, generally before septal positioning is attempted. Alternately, one can map the His area and perform pace mapping with the helix withdrawn, which give less chance to snag the tricuspid valvular apparatus. However, when performing pace mapping on the right side of the septum, unipolar impedances might be more accurate with extended helix and might allow a better reference impedance when screwing into the septum.
To avoid helix retraction when clockwise rotating the outer lead body, the inner coil of Solia S lead needs to be pretensioned before insertion. Therefore, the green stylet-guide is connected to the lead pin and pressed against the silicone coating at the proximal portion of the lead. To build up the torque on the inner coil, this green stylet-guide tool is rotated 8–10 times clockwise. As such, the inner coil builds up tension and rotations of the outer lead body are better transferred in a one-to-one relation to the inner coil and helix. This preparation step avoids unwanted helix retraction during screwing. To maintain the tension, the green stylet-guide is kept on the pin of the pacing lead while screwing the Solia S lead toward a deep septal position. Advancement of the Solia S lead into the septum is further facilitated by fast rotation (to overcome resistance at the right septal subendocardial layer) and by keeping the stylet advanced to the tip of the pacing lead. The stylet and stylet guide are kept in position until the final position is reached.
7.2. Ingevity Lead (Boston Scientific)
The Ingevity pacing lead (Boston Scientific Inc., Marlborough, MA, USA) is a 5.7 Fr diameter SDL with an extendable helix design. The electrically active helix is extended in advance using the standard clip-on-tool. To screw the Ingevity lead in a deep septal position two approaches are used. With the first approach, clockwise rotations on the outer lead body are applied. This generally leads to helix retraction, as described before, and further advancement in the septum becomes hampered, as the helix is no longer exposed. Helix retraction is often suggested by a sudden increase in pacing impedance (sometimes up to >2,000 Ohms). The helix needs to be extended once again using the clip-on-tool. Afterwards, new clockwise rotations on the outer lead body can be applied to further advance the lead. These maneuvers are repeated until a deep septal position is reached.
A second method consists in extending the helix in advance and fixating the helix and inner coil to the outer lead coil. As the stylet-guide tool of this lead does not get over the proximal silicone seal of the lead, the tension created on the inner coil is not maintained. However, a custom-made fixation tool can be made from an IS-1 lead-end cap (Gillis et al., 2021). First, the tip of an IS-1 lead end-cap is cut-off and the opened lead end-cap is slided over the proximal end of the pacing lead (beyond the proximal electrode). Secondly, with the stylet fully inserted in the lead, the stylet-guide tool is advanced onto the connector pin and around 15 rotations of the stylet-guide tool are applied to expose the helix and pretension the inner coil. Finally, without releasing the built-up tension, the lead-end cap is pulled back until the insertion tool is forced between the lead pin and the lead end cap. This technique allows to maintain the pretension on the inner coil and avoid helix retraction when clockwise rotations of the outer lead body of the Ingevity are applied. With both approaches the stylet remains advanced to the tip of the pacing lead while screwing as this facilitates lead advancement into the septum.
7.3. Tendril 2088TC (Abbott)
The Tendril 2088TC lead (Abbott, Inc., USA) is a 5.8 Fr SDL with an extended helix measuring 2 mm in length. The outer isolation of this lead consists of a polymer (OptimTM) made of silicone and polyurethane. This particular insulation has the potential to become damaged when subject to rotations applied on the outer lead body. Therefore, rotating the outer lead body of the Tendril is not recommended to obtain a deep septal position. However, the helix extension mechanism of this lead is protected from overturning and helix fracture has not been described, even with numerous rotations.
With the helix extended, the Tendril pacing lead is positioned at the right side of the septum and unipolar pace mapping is performed. The Tendril pacing lead is advanced into the septal tissue by continuous clockwise rotation of the connector pin using the standard clip-on-tool delivered with the lead. As the helix grips the septal tissue, continuous rotation of the lead pin will advance the helix and lead body further into the septum. The tapered transition between the helix and lead body facilitates the advancement of the Tendril lead in the septum. Often, 20–30 rotations on the lead pin are needed before the lead reaches the left side of the septum.
These specific techniques offer insights into handling different SDLs for LBBAP. For more detailed protocols, troubleshooting tips, and device-specific guidance, visit CONDUCT.EDU.VN, your trusted source for advanced cardiac pacing techniques, including right septal subendocardial layer, and helix extension mechanism.
8. Precautions and Potential Pitfalls of SDL-LBBAP
With the stylet inserted, SDL are stiffer than LLL and care must be taken not to perforate through the septum when implanting LBBAP leads. It is recommended to screw SDL in deep septal positions under fluoroscopic guidance and with continuous monitoring of the unipolar impedance and paced QRS. The lead implant depth can be assessed with contrast injection and based on the fluoroscopic landmarks of the pacing electrodes and interelectrode distance. As the lead advances into the septum, the unipolar pacing impedance tends to rise initially but decrease by 50–100 ohms as it approaches the left sided septal border. If the impedance drops by more than 200 ohms during screwing, further lead advancement is not recommended as this indicates that the helix is at the edge of the left sided septum. Absolute values of unipolar pacing impedance depend on the type, length, and design of the SDL. As the Boston Scientific Ingevity lead is developed as a high impedance pacing lead, it demonstrates higher unipolar impedances than the Tendril or the Solia S leads. Therefore, we recommend using unipolar pacing impedance at the right side of the septum as an individual reference for impedance monitoring during screwing. Furthermore, unipolar pacing impedances measured from the stylet are reported to be comparable to unipolar pacing impedances measured from the lead pin (Gillis et al., 2022).
A further potential pitfall of SDL is the risk of entanglement of the exposed helix in the right-sided subendocardial tissue. This so-called entanglement effect has previously been described in a cadaver model with LLL targeted to a deep septal position but can occur with any type of pacing lead (Jastrzebski et al., 2020). Entanglement of the helix occurs when the helix does not get grip on the septal tissue but instead becomes trapped in the septal subendocardial tissue. Prolonged rotation of the lead body without lead advancement into the septum, may eventually result in complete helix entrapment and difficulty in repositioning the lead (le Polain de Waroux et al., 2021). If entanglement is suspected, counter clockwise rotation and slight traction on the lead body while maintaining tension on the lead, usually untangles the lead. For expert guidance on preventing and managing these challenges, including helix entrapment and lead perforation, visit CONDUCT.EDU.VN.
9. Future Directions for LBBAP
Reported experience with LBBAP using SDL is limited (De Pooter et al., 2021; Zanon et al., 2020). In a recent study, SDL- and LLL-LBBAP yielded similar implant success rates, procedural safety and pacing characteristics (De Pooter et al., 2021). Although larger studies are needed to confirm these results, SDL may offer advantages for LBBAP for several reasons. The thicker lead body of SDL together with the support of the stylet results in excellent torquability and stiffness when targeting deep septal positions with rotations applied on the outer lead body effectively transferred to the distal part of the lead and helix. Compared to LLL, unwanted twisting of the lead at the entry of the delivery sheath during implant is rarely observed. Furthermore, the larger lead body diameter of SDL also allows for an improved tissue grip when rotating the lead body. As such, and despite the larger lead body diameter, SDL are characterized by an easy penetration into the septum.
Additionally, unipolar lead impedances can be monitored directly on the stylet of SDL, rather than through connection of the crocodile clamps on the lead pin (Gillis et al., 2022). This approach avoids repetitive connection and disconnection of the clamps, limits less lead body rotations, and offers continuous unipolar pacing and reliable impedance monitoring during screwing. Another advantage with stylet-driven leads is that in the unfortunate event of post-operative lead dislodgment, the lead may be repositioned in a “conventional” right ventricular position without having to regain venous access. Disadvantages include the requirement for lead preparation and particular precautions to avoid unwinding of the helix during deep septal lead positioning for SDL leads with extendable helices. An additional drawback is that His bundle pacing is generally easier with lumen-less leads, and in case LBBAP with SDL does not give satisfactory results, HBP as backup might not be as easy with SDL. Although, the optimal lead design for LBBAP (and CSP in general) has not yet been determined, several of the features of current SDL may merit incorporation into future dedicated LBBAP lead designs. Stay updated on the latest advancements in LBBAP technology and techniques by visiting CONDUCT.EDU.VN.
10. Conclusion
Mastering LBBAP with stylet-driven pacing leads requires a comprehensive understanding of lead designs, implantation techniques, and potential pitfalls. This guide provides a foundational overview to help you navigate the complexities of SDL-LBBAP. For more in-depth knowledge, device-specific protocols, and expert insights, turn to CONDUCT.EDU.VN, your ultimate resource for excellence in cardiac pacing.
Unlock the full potential of cardiac pacing with CONDUCT.EDU.VN, where you’ll find extensive resources on:
- Advanced Implantation Techniques: Step-by-step guides and video tutorials on LBBAP implantation.
- Troubleshooting and Complication Management: Expert advice on addressing common challenges during and after LBBAP procedures.
- Device-Specific Protocols: Detailed information on using different pacing leads and delivery systems.
- Continuing Education: Stay up-to-date with the latest research and best practices in cardiac pacing.
FAQ: Left Bundle Branch Area Pacing
-
What is Left Bundle Branch Area Pacing (LBBAP)?
LBBAP is a pacing technique that involves placing a lead deep into the ventricular septum to capture the left bundle branch, providing more physiological heart activation than traditional right ventricular pacing. -
Why is LBBAP considered better than Right Ventricular Pacing (RVP)?
LBBAP avoids the dyssynchrony associated with RVP, leading to improved cardiac function and reduced risk of heart failure. -
What are the main differences between Lumen-Less Leads (LLL) and Stylet-Driven Leads (SDL) for LBBAP?
LLL are thinner and lack a stylet, requiring a delivery sheath for support. SDL are wider, have a stylet for added stiffness, and often feature extendable-retractable helices. -
How is the Solia S lead prepared for LBBAP to prevent helix retraction?
The inner coil of the Solia S lead is pretensioned using a green stylet-guide tool, which is rotated clockwise to build up torque before insertion. -
What is the significance of monitoring unipolar pacing impedance during SDL-LBBAP?
Monitoring impedance helps assess the lead’s position in the septum; a sudden drop may indicate the lead is nearing the left-sided septal border. -
What is the “entanglement effect” and how can it be avoided?
The entanglement effect occurs when the helix gets trapped in the subendocardial tissue. It can be avoided by ensuring the helix grips the septal tissue and using counter clockwise rotation with slight traction if suspected. -
Can I use a standard IS-1 lead-end cap for the Ingevity lead to prevent helix retraction?
Yes, a custom-made fixation tool can be created from an IS-1 lead-end cap to maintain tension on the inner coil and prevent helix retraction during implantation. -
Why is rotating the outer lead body of the Tendril 2088TC lead not recommended?
The outer insulation of the Tendril 2088TC lead is prone to damage when subjected to rotations. Instead, the helix is advanced by continuous rotation of the connector pin. -
How do I differentiate left bundle branch pacing from left ventricular septal pacing on an ECG?
Left bundle branch pacing typically shows a narrow QRS morphology with a terminal r-wave in lead V1, indicating an incomplete right bundle branch block morphology. -
What should I do if LBBAP with SDL does not yield satisfactory results?
While His bundle pacing (HBP) is generally easier with lumen-less leads, consider alternative pacing strategies or consult with an experienced electrophysiologist to optimize outcomes.
For additional questions, contact us at:
CONDUCT.EDU.VN
100 Ethics Plaza, Guideline City, CA 90210, United States
Whatsapp: +1 (707) 555-1234
Website: conduct.edu.vn