Introduction
In health sciences research, theoretical frameworks are crucial for predicting and explaining health behavior, as well as for developing interventions that lead to better health outcomes. One such framework is the Health Belief Model (HBM), a social cognitive model that has been used in family planning research for decades. Soon after the introduction of the oral contraceptive pill (OC), professionals in reproductive health advocated for research grounded in theory to clarify inconsistent findings about factors related to contraceptive use and to guide the creation of more robust study designs. This article explores how the Health Belief Model can guide behavior in the context of contraceptive choices and family planning.
The Health Belief Model (HBM), a comprehensive social cognitive framework developed by Rosenstock and colleagues, has been used to predict and explain variations in contraceptive behavior among women. Despite its early application, the HBM has been seldom used in family planning research since then. Given the ongoing need for strategies to prevent unintended pregnancies and the evolved understanding of contraceptive behavior, it is worth re-examining the HBM as a framework for explaining and predicting modern contraceptive behavior. This review explores the suitability of the Health Belief Model (HBM) as a guide for understanding and influencing contraceptive decisions.
Methods
To examine the HBM framework, primary articles on the HBM in general and its constructs were used to provide an overview of the model. Articles included in this integrated review were primary research reports or editorials applying the HBM to family planning, specifically contraceptive behavior research. Relevant literature was identified using a computerized search for articles published from January 1966 through February 2011 using databases like MEDLINE, CINAHL, PubMed, Google Scholar, and PsychInfo. The keywords searched included combinations of “Health Belief Model,” “theory-guided research,” “health behavior theory,” AND “contraception,” “family planning,” “birth control,” and “contraceptive behavior.” This search strategy initially yielded 82 articles, of which ten were included in the review after applying inclusion/exclusion criteria.
Results
Overview of the Model
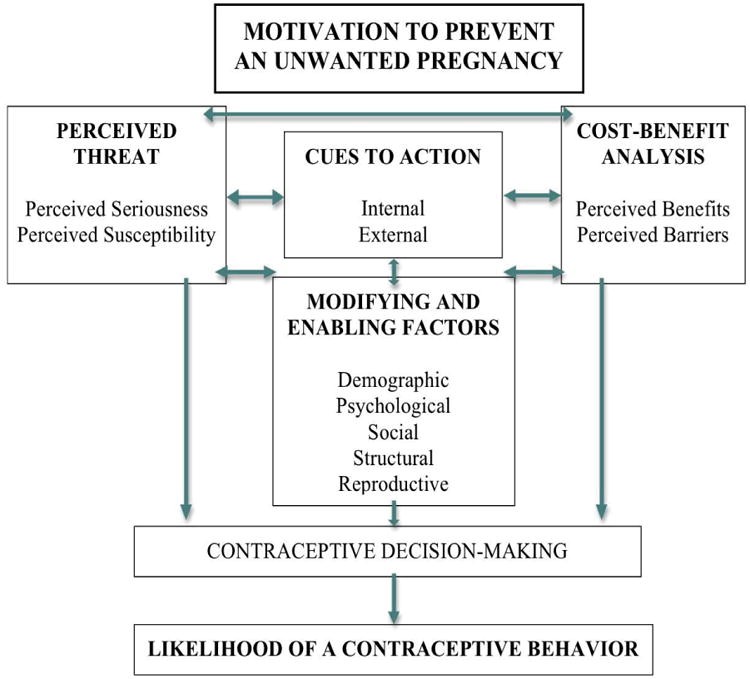
The Health Belief Model (HBM) is a cognitive, interpersonal framework that views people as rational beings who approach decision-making with a multi-faceted perspective regarding health behaviors. It is particularly suitable for complex preventive health behaviors, such as contraceptive behavior. The model is rooted in social psychology, emphasizing cognitive factors oriented towards achieving goals, like preventing pregnancy. Its constructs highlight modifiable factors, enabling interventions to address public health issues such as unintended pregnancies. Overall, the HBM’s adaptability makes it suitable for diverse contexts like family planning.
Family planning involves a dynamic set of services, programs, and behaviors aimed at regulating family size and spacing. Contraceptive behavior, a key aspect of family planning, includes activities involved in identifying and using contraceptive methods to prevent pregnancy. This can include contraceptive initiation, continuation, discontinuation, misuse, nonuse, compliance, and adherence.
Motivation to Prevent an Unwanted Pregnancy
Contraceptive behavior, viewed through the HBM, is driven by an individual’s:
- Desire to avoid pregnancy and the value placed on not becoming pregnant.
- Non-specific, stable differences in pregnancy motivations and childbearing desires.
- Perceived ability to control fertility and reduce the threat of pregnancy by using contraception.
Sufficient motivation is essential to make pregnancy prevention relevant and to support the contraceptive behavior decision-making process.
Key Constructs of Contraceptive Behavior
The constructs of the HBM, as applied to contraceptive behavior, are detailed below:
Perceived Threat
Perceived threat, encompassing both susceptibility and seriousness of an unwanted pregnancy and its potential consequences (birth, abortion, parenthood), serves as an incentive to use contraception. This construct considers personal feelings about the seriousness of becoming pregnant, based on a subjective assessment of medical and social consequences of pregnancy and childbearing. Factors such as fear of body changes or pregnancy complications, or concerns about quitting school or losing a job due to increased child-rearing responsibility, can impact the likelihood of contraceptive use.
Cost-Benefit Analysis
A crucial aspect of the Health Belief Model is the cost-benefit analysis individuals undertake when considering contraceptive options. This involves weighing perceived barriers against perceived benefits.
Perceived Barriers
Perceived barriers are negative consequences of using contraception. This includes potential side effects of hormonal contraception, physiological risks, inconvenience, and limited access to methods. All of these potential disadvantages can inhibit contraceptive use.
Perceived Benefits
Perceived benefits relate to the perceived effectiveness, feasibility, and other advantages of using a contraceptive method to prevent pregnancy vis-à-vis the perceived barriers. The perceived ratio of a contraceptive’s benefits to its barriers helps determine the preferred contraceptive action and method. This can also include non-contraceptive benefits, such as protection against certain cancers or improvement of menstrual symptoms.
Cues to Action
Cues to action are internal and external stimuli that trigger a consciousness of the perceived pregnancy threat and facilitate consideration of using contraception. This may include symptoms like missed menses or contraceptive communication from the media, and worry from a sexual partner or counseling by a health care provider.
Modifying and Enabling Factors
Modifying or enabling factors interact with an individual’s perceptions of pregnancy and decision-making to influence contraceptive use. This dimension includes demographic, social, structural, psychological, and reproductive factors.
Issues in Early Applications of the HBM for Family Planning
Early studies highlighted controversies over the applicability of the HBM for family planning due to inconsistencies in how contraceptive behavior was conceptualized. Some argued that the HBM was designed for “sick role” behaviors rather than preventive health behaviors, limiting its applicability in family planning since pregnancy is not a disease.
Evolving Contraceptive Research Provides for Enhanced HBM Applications
Advancements in family planning research and improved measurement of predictor and outcome variables have enabled more robust applications of the HBM to contraceptive behavior. Pregnancy prevention is now viewed as a health behavior in its own right, contributing to the maintenance and enhancement of physical, psychological, and social wellbeing.
Discussion
The Health Belief Model can be used to investigate the impact of new and improved contraceptive methods on behavior. Additionally, the HBM can guide the development, testing, and implementation of rigorously-designed contraceptive interventions that operationalize all HBM dimensions. Programs that are culturally- and health literacy-sensitive, employ multimodal learning strategies, and are evaluated using standardized techniques are warranted.
Implications for Research
Family planning researchers need to define and measure contraceptive outcomes carefully, customizing HBM applications to specific contraceptive behaviors and methods. More reliable measures of contraceptive use, such as serum and urine hormone concentrations and electronic monitoring devices, may contribute to more precise results and improve HBM applications.
Implications for Practice
Healthcare providers can use the HBM to understand patients’ contraceptive needs, employing its constructs to guide patient interviewing. The health history should focus not only on fertility intentions but also on perceptions of method-specific benefits and barriers, and on psychological, social, and reproductive histories. Health care professionals can structure contraceptive education and counseling sessions by the framework to ensure comprehensiveness of approach and content.
The HBM also offers a comprehensive approach to long-term patient contraceptive management plans, providing a structure for providers to reassess patients’ contraceptive behavior patterns and their dynamic needs within complex socioeconomic, environmental, and reproductive contexts.
Conclusion
The HBM provides a framework for predicting and explaining the complex systems of modern contraceptive behavior determinants and for promoting strategies to improve family planning outcomes. By understanding the factors that influence contraceptive choices, we can better guide behavior and improve reproductive health outcomes. The belief that can guide behavior, as embodied in the Health Belief Model, remains a powerful tool in family planning science and practice.