Cardiovascular disease (CVD) remains a leading cause of mortality worldwide, and despite advancements in medical care, the CVD mortality rate has plateaued, even showing signs of increasing. Poor dietary habits are a significant contributor to obesity and type 2 diabetes, both major risk factors for CVD. This article provides A Clinical Guide To Nutrition for healthcare professionals to effectively implement evidence-based dietary counseling in their practice.
While dietary modification is crucial for CVD prevention, its implementation in clinical settings is often hindered by inadequate nutrition training among clinicians. This guide reviews the key components of a heart-healthy diet, evidence-based dietary recommendations, and the impact of diet on CVD risk factor management. It also addresses the specific challenges of dietary counseling in low-socioeconomic-status (SES) populations, offering practical strategies to improve their access to healthier food choices.
The Building Blocks of a Heart-Healthy Diet
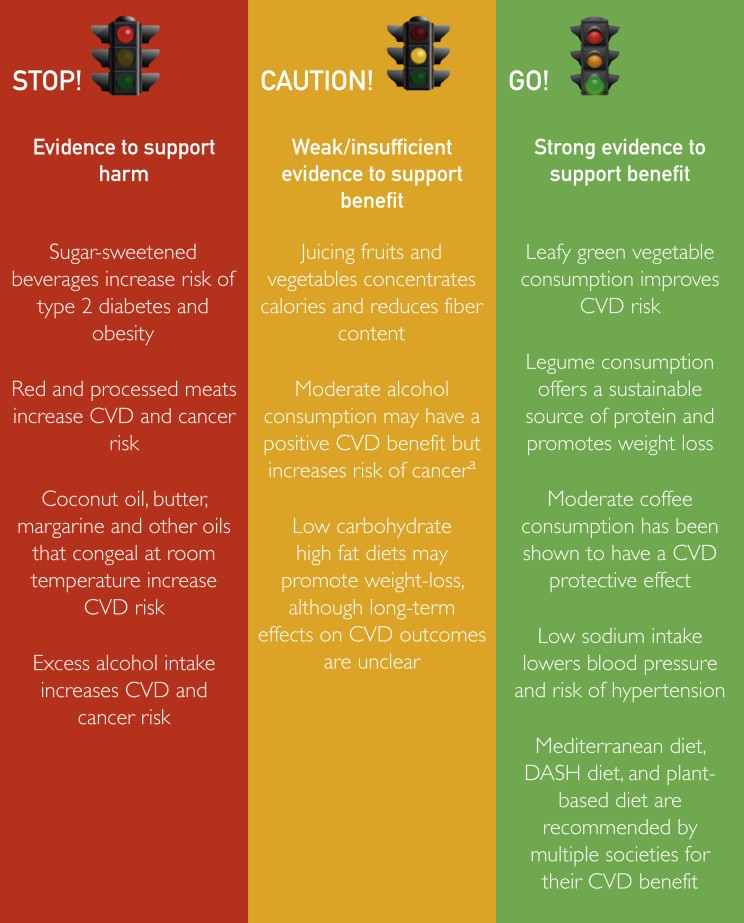
A healthy diet is rich in non-starchy vegetables, fruits, whole grains, and legumes, with moderate consumption of nuts, seafood, lean meats, low-fat dairy products, and vegetable oils. Conversely, trans-fats, saturated fats, sodium, red meat, refined carbohydrates, and sugar-sweetened beverages (SSBs) should be minimized or avoided.
Carbohydrates: Complex vs. Simple
Carbohydrates are a primary source of energy in most diets and can be categorized as complex or simple. Simple carbohydrates, found in refined grains and table sugar, are rapidly digested and absorbed, increasing the risk of type 2 diabetes, dyslipidemia, hypertension, CVD events, and mortality. Restricting consumption of high-fructose corn syrup is crucial due to its association with weight gain and elevated cholesterol levels.
Complex carbohydrates, present in legumes, whole grains, and starchy vegetables, offer sustained energy and essential nutrients. Whole grains, rich in fiber, lignans, and phytonutrients, promote satiety and have a lower glycemic index compared to refined grains.
Protein: Sources and Benefits
Legumes are a sustainable source of protein and fiber, contributing to weight loss and potentially reducing all-cause mortality. Nuts also provide valuable protein and fiber, and their consumption is linked to decreased LDL-C levels and reduced all-cause mortality.
Fats: Unsaturated vs. Saturated and Trans Fats
Dietary fats are classified as unsaturated (mono- and polyunsaturated), saturated, and trans-fats. Trans-fats pose the greatest risk to cardiovascular health, followed by saturated fats. Trans-fats, primarily found in partially hydrogenated oils, should be completely avoided. Saturated fats, present in processed foods, cheese, whole milk, butter, and margarine, should be limited to reduce LDL-C levels.
Vegetables and Fruits: Essential for Cardiovascular Health
Vegetables are essential for cardiovascular health, offering a low glycemic index profile and a wealth of beneficial micronutrients. Leafy green vegetables provide significant benefits through mechanisms like the conversion of inorganic nitrates to nitric oxide, promoting vascular health, and antioxidant and anti-inflammatory effects from carotenoids like lutein.
 Assortment of colorful fresh fruits and vegetables
Assortment of colorful fresh fruits and vegetables
Whole fruits are also integral to heart-healthy diets, providing antioxidant and anti-inflammatory benefits, promoting satiety, and generally having a low glycemic index. Berries, rich in anthocyanins, regulate endothelial function and glycemic metabolism.
Evidence-Based Dietary Patterns
Several dietary patterns have demonstrated significant cardiovascular benefits. The 2015-2020 Dietary Guidelines for Americans recommend three healthy eating patterns: the US healthy eating diet, the healthy Mediterranean diet, and the healthy vegetarian diet.
DASH Diet: A Proven Approach to Lowering Blood Pressure
The Dietary Approaches to Stop Hypertension (DASH) diet, originally developed to control hypertension, emphasizes fruits, vegetables, low-fat dairy, and limited sodium intake. Studies have shown that the DASH diet effectively lowers blood pressure, LDL-C levels, and overall cardiovascular risk.
Mediterranean Diet: Emphasizing Plant-Based Foods and Healthy Fats
The Mediterranean diet, based on traditional eating patterns in Southern Italy and Greece, is characterized by high intake of leafy green vegetables, fruits, whole grains, nuts, legumes, extra virgin olive oil, moderate intake of fish, lean meats, low-fat dairy, poultry, low intake of red meat and sweets, and moderate wine consumption. Adherence to the Mediterranean diet has been shown to lower both CHD and all-cause mortality.
Vegetarian Diet: A Plant-Based Approach to Cardiovascular Health
The vegetarian diet replaces meat, seafood, and poultry with soy products, legumes, nuts, and whole grains. This dietary pattern is associated with various health benefits, including reduced body mass index, non-HDL-C level, and SBP, in addition to lower risk for CVD.
Less Common Diets: Low-Carb & Keto
Low-carbohydrate, high-protein/fat (LCHF) diets, such as ketogenic, Atkins, and paleo diets, have gained popularity for weight loss. While they may improve weight loss and insulin sensitivity, they can also increase LDL-C levels. Currently, there is insufficient evidence to recommend LCHF diets for improving cardiovascular health, and long-term use may be associated with increased all-cause mortality.
Dietary Recommendations for Specific Conditions
Hypertension
Lifestyle interventions, including dietary changes, are critical for preventing and managing hypertension. Diets focused on reduced sodium intake, such as the DASH diet, effectively lower blood pressure. Increasing dietary potassium through potassium-rich fruits and vegetables can also have a blood pressure-lowering effect.
Hyperlipidemia
Limiting saturated fat and trans-fat intake is essential for managing hyperlipidemia. Substituting saturated fats with whole grains and healthy oils like extra virgin olive oil and canola oil can reduce MI, stroke, and risk for cardiovascular death.
Type 2 Diabetes Mellitus
Dietary interventions for type 2 diabetes focus on minimizing carbohydrate intake and prioritizing foods with a low glycemic index. The American Diabetes Association recommends moderate carbohydrate intake from vegetables, legumes, fruits, low-fat dairy, and whole grains, while reducing refined and added sugar intake.
Dietary Counseling: Practical Strategies for Clinicians
Effective dietary counseling begins with a lifestyle interview to assess the patient’s current eating habits, concerns, and readiness for change. Asking patients at least one question about nutrition and physical activity per visit can be a starting point. The ABCDs of “Assess, Barriers, Commit, and Demonstrate” can be used to understand opportunities for improved diet and activity.
Addressing Socioeconomic Barriers to Healthy Eating
Patients with low SES often face unique challenges in accessing healthy food choices. Food insecurity, long distances to supermarkets, and limited access to fresh foods can contribute to poor dietary habits. Clinicians should consider affordability and practicality when recommending dietary changes.
Conclusion: A Public Health Imperative
Improving dietary habits is a public health priority that can significantly reduce CVD morbidity and mortality. Clinicians must understand current dietary practice guidelines and implement evidence-based dietary counseling in those at high risk for CVD. By focusing on sustainable dietary changes and addressing individual patient needs and socioeconomic factors, clinicians can play a crucial role in promoting cardiovascular health.