Despite advances in healthcare, cardiovascular disease (CVD) mortality rates have stagnated, highlighting the critical role of modifiable risk factors like diet. Poor dietary habits contribute significantly to obesity and type 2 diabetes mellitus, both major drivers of CVD. This guide provides clinicians with an evidence-based approach to navigate trending cardiovascular nutrition controversies and implement effective dietary counseling in practice.
Dietary modification is a cornerstone of CVD prevention. However, its implementation is often hampered by inadequate nutrition training among clinicians. This review synthesizes current evidence on heart-healthy diets, addresses common nutritional controversies, and offers practical strategies for dietary counseling, particularly in low-socioeconomic-status (SES) settings.
The Foundation of a Heart-Healthy Diet
A heart-healthy diet emphasizes high consumption of fruits, non-starchy vegetables, whole grains, and legumes, alongside moderate intake of nuts, seafood, lean meats, low-fat dairy, and vegetable oils. Conversely, trans-fats, saturated fats, sodium, red meat, refined carbohydrates, and sugar-sweetened beverages (SSBs) should be minimized or avoided. The USDA’s MyPlate serves as a useful visual aid for patients.
Alt Text: USDA MyPlate visual guide depicting recommended daily intake proportions for fruits, vegetables, grains, protein foods, and dairy, promoting balanced nutrition.
Navigating Carbohydrate Choices
Carbohydrates, a significant part of most diets, are categorized as complex or simple. Simple carbohydrates, found in refined grains and table sugar, can increase the risk of type 2 diabetes, dyslipidemia, hypertension, and CVD. SSBs contribute substantially to added sugar intake and are linked to a dose-dependent increase in CVD risk. While diet sodas are often perceived as healthier alternatives, they have been associated with metabolic syndrome and may increase cravings for sweet, energy-dense foods. Encouraging water consumption is a preferable strategy.
Complex carbohydrates, present in legumes, whole grains, and starchy vegetables, offer sustained energy and essential nutrients. Whole grains are richer in fiber, lignans, and phytonutrients compared to refined grains, leading to increased satiety and a lower glycemic index. Legumes provide a cost-effective source of protein and fiber, promoting weight loss and potentially reducing all-cause mortality.
The Fat Debate: Saturated vs. Unsaturated
Dietary fats are classified into unsaturated (mono- and polyunsaturated), saturated, and trans-fats. Trans-fats pose the highest risk for adverse cardiovascular outcomes and should be eliminated entirely. Reducing saturated fat intake, commonly found in processed foods, cheese, and whole milk, is associated with lower LDL-C levels. Replacing saturated fats with polyunsaturated fatty acids yields the most significant improvements in lipid profiles.
Observational studies, such as the PURE study, have questioned conventional wisdom regarding saturated fat intake. However, limitations in study design and generalizability suggest that patients should still minimize consumption of both trans-fats and saturated fats, alongside reducing refined carbohydrates.
Dairy consumption’s impact on cardiovascular health remains a topic of debate. Meta-analyses suggest neutral or protective associations between certain dairy products (e.g., yogurt and cheese) and diabetes and CHD. Major guidelines still recommend moderate consumption of low-fat dairy due to concerns about LDL-C elevation and high caloric density.
Poultry, Seafood, and Red Meat: Finding the Right Balance
Guidelines generally recommend moderate intake of lean poultry and seafood, while limiting red meat consumption. Processed meats are associated with the greatest increase in CVD and cancer risk. Substituting red and processed meats with seafood, lean poultry, and nuts can reduce the risk of CHD. Fish, rich in omega-3 polyunsaturated fatty acids, offers significant cardiovascular benefits.
Coffee and Alcohol: Moderation is Key
Moderate coffee consumption (3-4 cups daily) has been linked to reduced all-cause mortality, decreased cancer risk, and a dose-dependent inverse relationship with the risk of developing type 2 diabetes. However, limiting added sugar and cream is crucial.
Alcohol consumption and CVD risk appear to have a U-shaped relationship, with moderate intake potentially offering some benefit. However, recent research suggests that any level of alcohol consumption increases the risk of all-cause mortality and cancer. Current evidence does not support recommending alcohol consumption initiation for those who abstain.
Evidence-Based Dietary Patterns: DASH, Mediterranean, and Vegetarian
Clinicians should emphasize diets with strong evidence supporting cardiovascular benefits. The Mediterranean and DASH diets are associated with reduced mortality from CHD, CVD, and all causes.
The DASH diet, originally designed to control hypertension, emphasizes fruits, vegetables, whole grains, and low-fat dairy, while limiting saturated fat, cholesterol, and sodium. The Mediterranean diet, based on traditional eating patterns from Southern Italy and Greece, prioritizes high intake of leafy green vegetables, fruits, whole grains, nuts, legumes, and extra virgin olive oil, alongside moderate intake of fish, lean meats, low-fat dairy, and poultry.
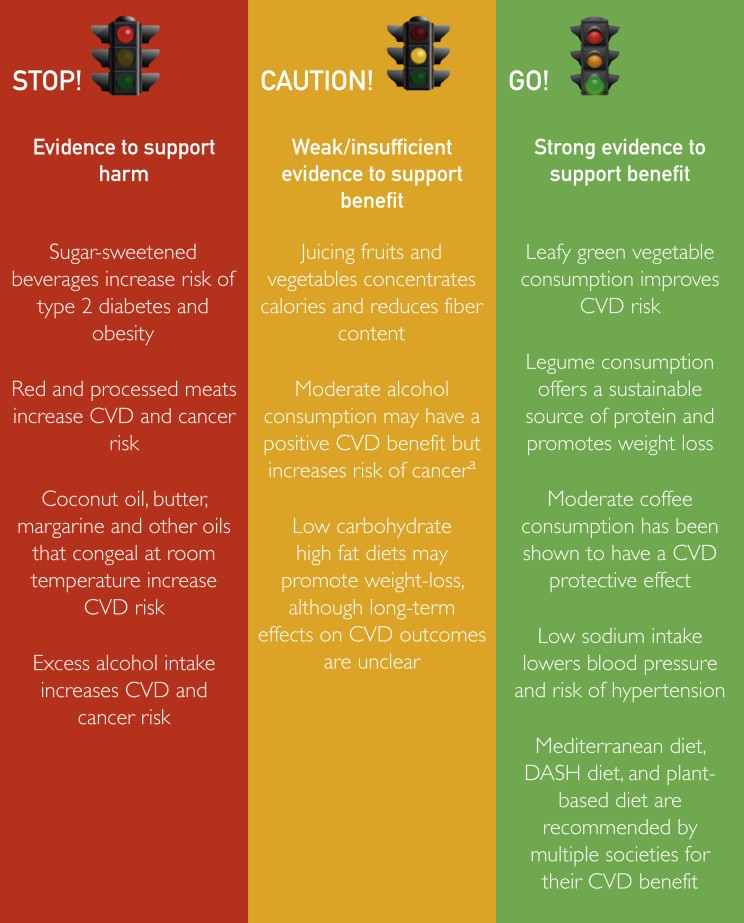 Dietary intervention impact on cardiovascular health
Dietary intervention impact on cardiovascular health
Alt Text: The figure shows a classification of dietary interventions and their corresponding impact on cardiovascular health, distinguishing interventions supported by evidence of benefit versus harm.
Vegetarian diets, which substitute meat, seafood, and poultry with soy products, legumes, nuts, and whole grains, offer various health benefits, including reduced body mass index, non-HDL-C levels, SBP, and CVD risk. Vegan diets, eliminating all animal-derived products, require vitamin B12 and D supplementation due to the risk of deficiency.
Addressing the Low-Carb Trend: LCHF Diets
Low-carbohydrate, high-protein/fat (LCHF) diets like ketogenic, Atkins, and paleo diets have gained popularity. While they may improve weight loss and insulin sensitivity, they can also increase LDL-C levels. Long-term adherence to LCHF diets emphasizing animal fat and protein may be associated with increased all-cause mortality. Currently, there is insufficient evidence to recommend LCHF diets for cardiovascular health improvement, however, increased intake of green leafy vegetables and plant-based proteins should be encouraged in individuals that pursue an LCHF diet.
Practical Dietary Counseling Strategies
Effective dietary counseling requires a personalized approach that considers individual needs, preferences, and limitations. A brief lifestyle interview can help assess current dietary habits, identify barriers to change, and set realistic goals. Integrating questions about nutrition and physical activity into routine clinical visits is a practical starting point.
Addressing Socioeconomic Disparities
Socioeconomic disparities significantly impact diet quality. Food insecurity and limited access to supermarkets offering fresh foods (“food deserts”) can hinder dietary improvements. Time constraints and limited resources can also lead to reliance on unhealthy processed and fast foods.
Providers should inquire about affordability and cost-effectiveness when counseling patients on healthy diets. Recommending affordable alternatives like frozen or canned fruits, vegetables, and legumes can promote access to nutritious options.
Conclusion: A Team-Based Approach to Cardiovascular Nutrition
In conclusion, effective dietary counseling is crucial for addressing the obesity epidemic and improving cardiovascular outcomes. The DASH diet, Mediterranean diet, and vegetarian diet are the most evidence-based approaches for CVD prevention and weight loss. A team-based approach, involving nurses and dietitians, can enhance education and reinforce healthy dietary habits. Addressing socioeconomic barriers and tailoring recommendations to individual circumstances is essential for achieving sustainable dietary changes and improving cardiovascular health for all patients.
