This guide provides a comprehensive overview for clinicians on the prevention, diagnosis, and treatment of osteoporosis. Developed by the National Osteoporosis Foundation (NOF), in collaboration with experts in bone health, this resource offers evidence-based recommendations for managing osteoporosis in postmenopausal women and men aged 50 and older.
Executive Summary: Understanding and Addressing Osteoporosis
Osteoporosis, often undetected until fractures occur, poses a significant health burden due to the aging population. These fractures, resulting from minimal or no trauma, impact individuals and place a substantial economic strain on healthcare systems. This guide emphasizes the importance of early intervention through prevention, accurate diagnosis, and effective treatment to mitigate the risk of fractures.
Since the initial NOF guide in 1999, it’s evident that many patients lack sufficient information on osteoporosis prevention and are not receiving appropriate diagnostic testing. A critical concern is the underdiagnosis and undertreatment of individuals who have already experienced osteoporosis-related fractures.
This clinician’s guide offers practical recommendations for preventing, assessing risk, diagnosing, and treating osteoporosis in postmenopausal women and men over 50. It includes guidelines for bone densitometry and fracture risk thresholds, informing decisions about pharmacologic interventions. The treatment recommendations are supported by cost-effectiveness analyses.
Key Recommendations for Clinicians
The following recommendations are for postmenopausal women and men aged 50 and older.
Universal Recommendations
- Counseling: Educate patients on the risks of osteoporosis and associated fractures.
- Calcium Intake: Recommend adequate daily calcium intake (1000 mg for men 50-70; 1200 mg for women 51+ and men 71+), supplementing if necessary.
- Vitamin D Intake: Advise on vitamin D intake (800–1000 IU/day), including supplements for individuals aged 50 and older.
- Exercise: Encourage regular weight-bearing and muscle-strengthening exercises to improve agility, strength, posture, and balance, thereby reducing falls and fractures.
- Fall Risk Assessment: Evaluate fall risk factors and suggest modifications (e.g., home safety assessments, balance training, vitamin D correction, medication review, vision correction).
- Lifestyle: Counsel on smoking cessation and limiting alcohol consumption.
Diagnostic Assessment
-
Height Measurement: Measure height annually, preferably using a stadiometer.
-
Bone Mineral Density (BMD) Testing: Conduct BMD testing:
- In women aged 65 and older and men aged 70 and older.
- In postmenopausal women and men aged 50-69, based on risk factor profiles.
- In adults aged 50 and older who have experienced a fracture, to diagnose and determine the severity of osteoporosis.
- Utilize dual-energy X-ray absorptiometry (DXA) with quality assurance measures.
-
Vertebral Imaging: Perform vertebral imaging:
-
In women aged 70 and older and men aged 80 and older with a BMD T-score ≤−1.0 at the spine, hip, or femoral neck.
-
In women aged 65-69 and men aged 70-79 with a BMD T-score ≤−1.5 at the spine, hip, or femoral neck.
-
In adults aged 50 and older with specific risk factors:
- Low-trauma fracture in adulthood (50+).
- Height loss (historical: ≥1.5 in. or 4 cm; prospective: ≥0.8 in. or 2 cm).
- Current or long-term glucocorticoid treatment.
-
Consider vertebral imaging based on age alone, if bone density testing isn’t available.
-
-
Secondary Causes: Investigate potential secondary causes of osteoporosis.
-
Biochemical Markers: Use bone turnover markers to aid risk assessment and monitor treatment.
Patient Monitoring
- BMD Testing: Repeat BMD testing 1-2 years after starting osteoporosis treatment, then every 2 years.
- More frequent testing may be needed in specific cases.
- Longer intervals between screenings may be appropriate for low-risk patients with normal or upper-low bone mass T-scores.
- Biochemical Markers: Repeat biochemical marker testing to assess treatment efficacy.
Pharmacologic Treatment Recommendations
- Initiate Treatment: Consider pharmacologic treatment:
- In patients with hip or vertebral fractures (clinical or asymptomatic).
- In those with T-scores ≤−2.5 at the femoral neck, hip, or lumbar spine by DXA.
- In postmenopausal women and men aged 50 and older with low bone mass (T-score between −1.0 and −2.5) and a 10-year hip fracture probability ≥3 % or a major osteoporosis-related fracture probability ≥20 % based on the FRAX® tool.
- FDA-Approved Therapies: Approved options include bisphosphonates (alendronate, ibandronate, risedronate, zoledronic acid), calcitonin, estrogen agonist/antagonist (raloxifene), estrogens and/or hormone therapy, tissue-selective estrogen complex (conjugated estrogens/bazedoxifene), parathyroid hormone 1–34 (teriparatide), and RANK ligand inhibitor (denosumab).
- Treatment Duration: Reassess risk after the initial treatment period; no pharmacologic therapy should be considered indefinite in duration.
- Post-Fracture Care: Implement risk assessment and treatment measures after a fracture, and consider fracture liaison service (FLS) programs.
Osteoporosis: Impact and Overview
Scope of the Problem
Osteoporosis is a widespread bone disease characterized by low bone mass, deterioration of bone tissue, compromised bone strength, and increased fracture risk. Diagnosed via BMD testing at the hip or lumbar spine, osteoporosis is indicated by a score 2.5 standard deviations below the young-adult reference population mean. Fractures occur most frequently in individuals with low bone mass.
It affects millions of people of all sexes and races, with prevalence increasing as populations age. NOF estimates that over 9.9 million Americans have osteoporosis, and an additional 43.1 million have low bone density. Roughly half of Caucasian women and one in five men will experience an osteoporosis-related fracture.
Medical Impact
Fractures, particularly of the vertebrae, hip, and forearm, are the primary clinical consequence of osteoporosis. Even fractures resulting from considerable trauma in older adults are often related to low bone mass. A recent fracture in an adult over 50 should prompt further assessment and treatment. Fractures can lead to chronic pain, disability, and mortality.
Hip fractures are associated with an 8-36% excess mortality within one year and a 2.5-fold increased risk of future fractures. A significant percentage of hip fracture patients require long-term nursing home care, with only a minority fully regaining their pre-fracture independence. Vertebral fractures, even silent ones, can cause pain, disability, deformity, and mortality. Wrist fractures can interfere with daily activities.
Economic Toll
Osteoporosis leads to two million fractures annually in the USA, causing substantial hospital admissions, medical office visits, and nursing home admissions. Medicare covers a significant portion of these costs, with hip fractures accounting for most expenditure. Costs are projected to rise to $25.3 billion by 2025.
Despite effective treatments, only a minority of women aged 67 or older who experience an osteoporosis-related fracture receive appropriate testing or treatment within six months after the fracture.
Basic Pathophysiology
Bone mass in older adults is the peak bone mass achieved in early adulthood, minus the amount of bone subsequently lost. Peak bone mass is influenced by genetic factors, nutrition, endocrine status, physical activity, and overall health during growth.
Bone remodeling removes older bone and replaces it with new bone. Bone loss occurs when bone removal exceeds replacement, particularly during menopause and advancing age. This imbalance leads to disordered skeletal architecture and increased fracture risk.
Individual trabecular plates of bone are lost, leaving a weakened structure with reduced mass. Rapid bone remodeling increases bone fragility and fracture risk.
Factors associated with increased osteoporosis-related fracture risk include aging, sex steroid deficiency, glucocorticoid use, and reduced bone quality. Fractures occur when weakened bone is overloaded, often by falls or activities of daily living.
 Pathogenesis of osteoporosis-related fractures
Pathogenesis of osteoporosis-related fractures
Approach to the Diagnosis and Management of Osteoporosis
NOF recommends a comprehensive approach to osteoporosis diagnosis and management, incorporating history, physical examination, BMD assessment, vertebral imaging, and fracture probability estimation. Therapeutic intervention thresholds are based on cost-effectiveness analyses. Clinicians use their skills and experience, along with patient-based research, to determine appropriate therapeutic interventions, discussing potential risks and benefits with patients.
Risk Assessment
All postmenopausal women and men aged 50 and older should be evaluated for osteoporosis risk. The more risk factors present, the greater the fracture risk. Osteoporosis is preventable and treatable, but often undiagnosed until a fracture occurs. Risk factors include lifestyle factors, genetic diseases, hypogonadal states, endocrine disorders, gastrointestinal disorders, hematologic disorders, rheumatologic and autoimmune diseases, neurological and musculoskeletal risk factors, miscellaneous conditions and diseases, and medications.
Since most osteoporosis-related fractures result from falls, it’s crucial to assess fall risk factors like history of falling, muscle weakness, gait abnormalities, selected medications, balance issues, and visual deficits.
Several risk factors are included in the WHO 10-year fracture risk model (FRAX®), which increases fracture risk independent of BMD. This model combines BMD measurements with clinical risk factors to assess individual patient risk.
Diagnostic Assessment
Consider osteoporosis and fracture risk based on risk factors and conditions. Rule out other metabolic bone diseases. Obtain relevant blood and urine studies if a secondary cause is suspected. Evaluate any adulthood fracture for osteoporosis. Recent fractures signify increased fracture risk. Patients with recent fractures, multiple fractures, or very low BMD should be evaluated for secondary etiologies.
Osteoporosis affects men; therefore, screening recommendations for men are outlined in Table 8.
Diagnosis
Diagnose osteoporosis via BMD measurement or adulthood hip or vertebral fracture without major trauma. Exclude secondary causes through laboratory testing.
BMD Measurement and Classification
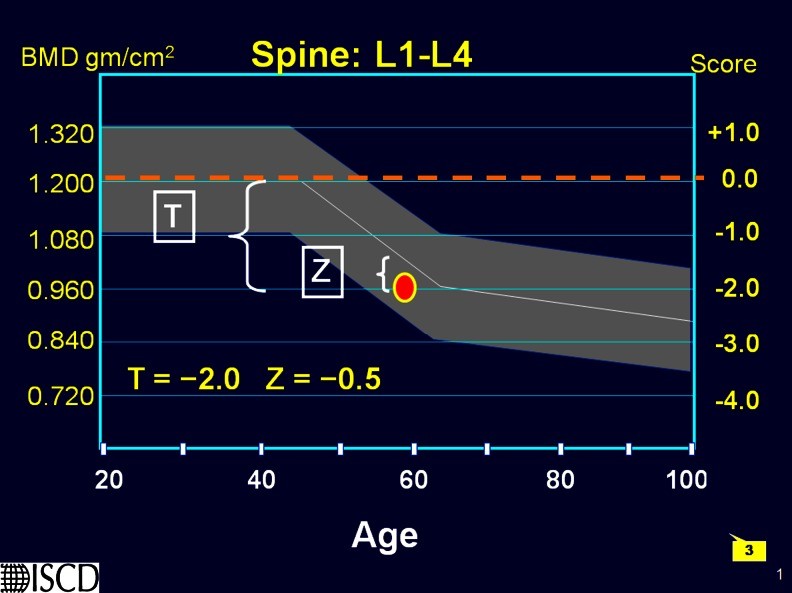
DXA is used to establish or confirm osteoporosis, predict fracture risk, and monitor patients. BMD is expressed as grams of mineral per square centimeter (g/cm2) and as T-scores and Z-scores. T-scores compare BMD to a young-adult reference population, while Z-scores compare BMD to an age-, sex-, and ethnicity-matched population.
An individual’s BMD is presented as the standard deviation above or below the mean BMD of the reference population, as outlined in Table 5. The BMD diagnosis of normal, low bone mass (osteopenia), osteoporosis, and severe or established osteoporosis is based on the WHO diagnostic classification.
BMD correlates with bone strength and predicts fracture risk. Fracture risk increases exponentially as BMD decreases. DXA at the hip is the best predictor of hip fracture risk. Lumbar spine and hip DXA measurements must be performed by trained technologists on properly maintained instruments.
The WHO diagnostic T-score criteria are applied to lumbar spine and femoral neck BMD measurements in postmenopausal women and men aged 50 and older. DXA at the one-third radius site can be used when hip and lumbar spine measurements are not possible. WHO BMD diagnostic classification should not be applied to premenopausal women, men under 50, and children.
Who Should Be Tested?
Base the decision to perform bone density assessment on individual fracture risk profiles and skeletal health assessments. Bone density measurement is indicated only if the results will influence treatment decisions. The US Preventive Services Task Force recommends testing all women aged 65 and older and younger women with fracture risk equal to or greater than that of a 65-year-old white woman without additional risk factors.
BMD measurement is not recommended in children or adolescents and not routinely indicated in healthy young men or premenopausal women unless significant fracture history or specific risk factors for bone loss exist.
Vertebral Imaging
A vertebral fracture is consistent with osteoporosis, even without a bone density diagnosis, indicating pharmacologic treatment. Vertebral imaging diagnoses asymptomatic fractures. Radiographically confirmed vertebral fractures are strong predictors of new fractures. Vertebral imaging can be performed via lateral thoracic and lumbar spine X-ray or lateral vertebral fracture assessment (VFA) on DXA machines.
Indications for Vertebral Imaging
Vertebral imaging is recommended based on age and BMD T-score, with consideration of specific risk factors.
Biochemical Markers of Bone Turnover
Biochemical markers of bone remodeling may predict fracture risk independently of bone density, predict the rapidity of bone loss, and predict extent of fracture risk reduction when repeated after 3–6 months of treatment with FDA-approved therapies
Use of WHO FRAX® in the USA
FRAX® calculates the 10-year probability of hip fracture and major osteoporotic fracture, considering femoral neck BMD and clinical risk factors. It is calibrated to US fracture and mortality rates.
The WHO algorithm used in this Guide was calibrated to US fracture and mortality rates; therefore, the fracture risk figures herein are specific for the US population. Economic modeling was performed to identify the 10-year hip fracture risk above which it is cost-effective, from the societal perspective, to treat with pharmacologic agents.
FRAX underestimates fracture risk in patients with recent fractures, multiple osteoporosis-related fractures, and those at increased risk for falling. FRAX® is most useful in patients with low femoral neck BMD. Utilizing FRAX® in patients with low BMD at the lumbar spine but a relatively normal BMD at the femoral neck underestimates fracture risk in these individuals. Specifically, the WHO algorithm has not been validated for the use of lumbar spine BMD. NOF recommends treatment of individuals with osteoporosis of the lumbar spine as well as the hip.
Additional Bone Densitometry Technologies
Additional bone mass measurement technologies included in Table 8 are capable of predicting both site-specific and overall fracture risk.
Universal Recommendations for All Patients
Recommend interventions to preserve bone strength, including adequate calcium and vitamin D intake, regular weight-bearing and muscle-strengthening exercise, smoking cessation, alcoholism identification and treatment, and fall risk factor treatment.
Adequate Intake of Calcium and Vitamin D
Adequate daily calcium and vitamin D intake is a safe and inexpensive way to reduce fracture risk. A balanced diet rich in low-fat dairy products, fruits, and vegetables provides calcium. Calcium supplements should be used when an adequate dietary intake cannot be achieved.
Lifelong adequate calcium intake is necessary for the acquisition of peak bone mass and subsequent maintenance of bone health. The skeleton contains 99 % of the body’s calcium stores; when the exogenous supply is inadequate, bone tissue is resorbed from the skeleton to maintain serum calcium at a constant level.
NOF supports Institute of Medicine (IOM) recommendations that men age 50–70 consume 1000 mg/day of calcium and that women age 51 and older and men age 71 and older consume 1200 mg/day of calcium.
Vitamin D plays a major role in calcium absorption, bone health, muscle performance, balance, and risk of falling. NOF recommends an intake of 800 to 1000 international units (IU) of vitamin D per day for adults age 50 and older.
Many older patients are at high risk for vitamin D deficiency. Serum 25(OH)D levels should be measured in patients at risk of deficiency. Vitamin D supplements should be recommended in amounts sufficient to bring the serum 25(OH)D level to approximately 30 ng/ml (75 nmol/L) and a maintenance dose recommended to maintain this level, particularly for individuals with osteoporosis. Many patients with osteoporosis will need more than the general recommendation of 800–1000 IU/day.
Treatment of Vitamin D Deficiency
Adults who are vitamin D deficient may be treated with 50,000 IU of vitamin D2 or vitamin D3 once a week or the equivalent daily dose (7000 IU vitamin D2 or vitamin D3) for 8–12 weeks to achieve a 25(OH)D blood level of approximately 30 ng/ml. This regimen should be followed by maintenance therapy of 1500–2000 IU/day or whatever dose is needed to maintain the target blood level.
Regular Weight-Bearing and Muscle-Strengthening Exercise
Recommend regular weight-bearing and muscle-strengthening exercise to reduce the risk of falls and fractures. Weight-bearing exercise includes walking, jogging, Tai Chi, stair climbing, dancing, and tennis. Muscle-strengthening exercise includes weight training and other resistive exercises, such as yoga, Pilates, and boot camp programs. Before an individual with osteoporosis initiates a new vigorous exercise program, such as running or heavy weight-lifting, a clinician’s evaluation is appropriate.
Fall Prevention
Implement strategies to reduce falls, including multifactorial interventions like individual risk assessment, exercise programs, home safety assessment and modification, and gradual withdrawal of psychotropic medication if possible. Appropriate correction of visual impairment may improve mobility and reduce risk of falls.
There is a lack of evidence that the use of hip protectors by community-dwelling adults provides statistically significant reduction in the risk of hip or pelvis fractures. Also, there is no evidence that the use of hip protectors reduces the rate of falls.
Cessation of Tobacco Use and Avoidance of Excessive Alcohol Intake
Advise patients to stop tobacco smoking. NOF strongly encourages a smoking cessation program as an osteoporosis intervention.
Recognize and treat patients with excessive alcohol intake. Moderate alcohol intake has no known negative effect on bone and may even be associated with slightly higher bone density and lower risk of fracture in postmenopausal women. However, alcohol intake of more than two drinks per day for women or three drinks a day for men may be detrimental to bone health, increases the risk of falling, and requires further evaluation for possible alcoholism.
Pharmacologic Therapy
All patients being considered for treatment of osteoporosis should also be counseled on risk factor reduction including the importance of calcium, vitamin D, and exercise as part of any treatment program for osteoporosis. Prior to initiating treatment, patients should be evaluated for secondary causes of osteoporosis and have BMD measurements by central DXA, when available, and vertebral imaging studies when appropriate. Biochemical marker levels should be obtained if monitoring of treatment effects is planned.
Who Should Be Considered for Treatment?
Postmenopausal women and men age 50 and older presenting with the following should be considered for treatment:
Although FRAX calculated fracture risk prediction has been confirmed in multiple studies, there are relatively few data confirming fracture risk reductions with pharmacotherapy in this group of patients.
US FDA-Approved Drugs for Osteoporosis
Current FDA-approved pharmacologic options for the prevention and/or treatment of postmenopausal osteoporosis include, in alphabetical order: bisphosphonates (alendronate, alendronate plus D, ibandronate, risedronate and zoledronic acid), calcitonin, estrogens (estrogen and/or hormone therapy), estrogen agonist/antagonist (raloxifene), tissue-selective estrogen complex (conjugated estrogens/bazedoxifene), parathyroid hormone (PTH [1–34], teriparatide), and the receptor activator of nuclear factor kappa-B (RANK) ligand (RANKL) inhibitor denosumab.
Bisphosphonates
Drug Efficacy
Alendronate reduces the incidence of spine and hip fractures by about 50 % over 3 years in patients with a prior vertebral fracture or in patients who have osteoporosis at the hip site. It reduces the incidence of vertebral fractures by 48 % over 3 years in patients without a prior vertebral fracture.
Ibandronate reduces the incidence of vertebral fractures by about 50 % over 3 years, but reduction in risk of nonvertebral fracture with ibandronate has not been documented
Risedronate reduces the incidence of vertebral fractures by 41 to 49 % and nonvertebral fractures by 36 % over 3 years, with significant risk reduction occurring within 1 year of treatment in patients with a prior vertebral fracture.
Zoledronic acid reduces the incidence of vertebral fractures by 70 % (with significant reduction at 1 year), hip fractures by 41 %, and nonvertebral fractures by 25 % over 3 years in patients with osteoporosis defined by prevalent vertebral fractures and osteoporosis by BMD of the hip.
Drug Administration
Alendronate and risedronate tablets must be taken on an empty stomach, first thing in the morning, with 8 oz of plain water. Delayed release risedronate tablets must be taken immediately after breakfast with at least 4 oz of plain water. Ibandronate must be taken on an empty stomach, first thing in the morning, with 8 oz of plain water.
Zoledronic acid, 5 mg in 100 ml, is given once yearly or once every 2 years by intravenous infusion over at least 15 min.
Drug Safety
Side effects are similar for all oral bisphosphonate medications and include gastrointestinal problems such as difficulty swallowing and inflammation of the esophagus and stomach.
All bisphosphonates can affect renal function and are contraindicated in patients with estimated GFR below 30–35 ml/min. Eye inflammation can also occur. There have been rare reports of osteonecrosis of the jaw (ONJ) with long-term use of bisphosphonates for osteoporosis, though ONJ is much more common following high-dose intravenous bisphosphonate treatment for patients with cancer. The risk of ONJ appears to increase with duration of treatment beyond 5 years.
Although rare, low-trauma atypical femur fractures may be associated with the long-term use of bisphosphonates (e.g., >5 years of use).
Calcitonin
Drug Efficacy
Calcitonin reduces vertebral fracture occurrence by about 30 % in those with prior vertebral fractures but has not been shown to reduce the risk of nonvertebral fractures. Due to the possible association between malignancy and calcitonin-salmon use, the need for continued therapy should be re-evaluated on a periodic basis.
Drug Administration
Two hundred international units delivered as a single daily intranasal spray. Subcutaneous administration by injection also is available.
Drug Safety
Intranasal calcitonin can cause rhinitis, epistaxis, and allergic reactions, particularly in those with a history of allergy to salmon.
Estrogen/Hormone Therapy (ET/HT)
Drug Efficacy
The Woman’s Health Initiative (WHI) found that 5 years of HT (Prempro®) reduced the risk of clinical vertebral fractures and hip fractures by 34 % and other osteoporotic fractures by 23 %.
Drug Administration
ET/HT is available in a wide variety of oral as well as transdermal preparations including estrogen only, progestin only, and combination estrogen–progestin.
Drug Safety
The WHI reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis during 5 years of treatment with conjugated equine estrogen and medroxyprogesterone acetate (Prempro®). Subsequent analyses of these data showed no increase in cardiovascular disease in women starting treatment within 10 years of menopause. Because of the risks, ET/HT should be used in the lowest effective doses for the shortest duration to treat moderately severe menopausal symptoms and should be considered primarily for women within the first few years of menopause.
Estrogen Agonist/Antagonist (Formerly Known as SERMs): Raloxifene
Drug Efficacy
Raloxifene reduces the risk of vertebral fractures by about 30 % in patients with a prior vertebral fracture and by about 55 % in patients without a prior vertebral fracture over 3 years. Reduction in risk of nonvertebral fracture with raloxifene has not been documented. Raloxifene is also indicated for the reduction in risk of invasive breast cancer in postmenopausal women with osteoporosis. Raloxifene does not reduce the risk of coronary heart disease.
Drug Administration
Available in a 60-mg tablet form to be taken with or without food.
Drug Safety
Raloxifene increases the risk of deep vein thrombosis to a degree similar to that observed with estrogen. It can also increase hot flashes and cause leg cramps.
Tissue-Selective Estrogen Complex: Conjugated Estrogens/Bazedoxifene (Conjugated Estrogens Paired with Estrogen Agonist/Antagonist)
Drug Efficacy
Conjugated estrogens/bazedoxifene significantly increased mean lumbar spine BMD (treatment difference, 1.51 %), at 12 months compared to placebo in women who had been postmenopausal between 1 and 5 years. Treatment with conjugated estrogens/bazedoxifene also increased total hip BMD. The treatment difference in total hip BMD at 12 months was 1.21 %.
Drug Administration
Available as a tablet containing conjugated estrogens and bazedoxifene 0.45 mg/ 20 mg, to be taken once daily without regard to meals.
Drug Safety
Side effects of conjugated estrogens/bazedoxifene include muscle spasms, nausea, diarrhea, dyspepsia, upper abdominal pain, oropharyngeal pain, dizziness, and neck pain.
Parathyroid Hormone: Teriparatide
Drug Efficacy
Teriparatide reduces the risk of vertebral fractures by about 65 % and nonvertebral fragility fractures by about 53 % in patients with osteoporosis, after an average of 18 months of therapy.
Drug Administration
Teriparatide is an anabolic (bone-building) agent administered by 20 μg daily subcutaneous injection. Treatment duration is recommended not to exceed 18 to 24 months.
Drug Safety
Side effects of teriparatide include leg cramps, nausea, and dizziness.
RANKL/RANKL Inhibitor: Denosumab
Drug Efficacy
Denosumab reduces the incidence of vertebral fractures by about 68 %, hip fractures by about 40 %, and nonvertebral fractures by about 20 % over 3 years.
Drug Administration
Administered by a health professional, 60 mg every 6 months as a subcutaneous injection.
Drug Safety
Denosumab may cause hypocalcemia. Denosumab increased the risk of serious skin infections (cellulitis) and skin rash.
Sequential and Combination Therapy
Sequential treatment with anabolic therapy followed by an antiresorptive agent is generally preferred to concomitant combination therapy.
Duration of Treatment
No pharmacologic therapy should be considered indefinite in duration. After the initial 3- to 5-year treatment period, a comprehensive risk assessment should be performed. It is reasonable to discontinue bisphosphonates after 3 to 5 years in people who appear to be at modest risk of fracture after the initial treatment period. In contrast, for those who appear to be at high risk for fracture, continued treatment with a bisphosphonate or an alternative therapy should be considered.
Monitoring Patients
Accurate yearly height measurement is a critical determination of osteoporosis treatment efficacy. Serial central DXA testing is an important component of osteoporosis management.
The following techniques may be used to monitor the effectiveness of treatment: Central DXA, QCT, pDXA, pQCT, and QUS and Biochemical markers of bone turnover
Implementation of FLS Secondary Fracture Prevention Programs
FLS programs have accomplished a reduction in secondary fracture rates as well as health care cost savings. A Fracture Liaison Service is a coordinated care system headed by an FLS coordinator who ensures that individuals who suffer a fracture receive appropriate diagnosis, treatment, and support.
Physical Medicine and Rehabilitation
Physical medicine and rehabilitation can reduce disability, improve physical function, and lower the risk of subsequent falls in patients with osteoporosis. Rehabilitation and exercise are recognized means to improve function, such as activities of daily living. Psychosocial factors also strongly affect functional ability of the patient with osteoporosis who has already suffered fractures.
Conclusions and Remaining Questions
This Guide has focused on the prevention, diagnosis, and treatment of osteoporosis in postmenopausal women and men age 50 and older using the most common existing diagnostic and treatment methods available. Many additional issues urgently need epidemiologic, clinical, and economic research.
NOF is committed to continuing the effort to answer these and other questions related to this debilitating disease, with the goal of eliminating osteoporosis as a threat to the health of present and future generations. For additional resources on osteoporosis and bone health, visit www.nof.org.