Nuclear medicine offers invaluable insights into organ function and disease processes, complementing the structural information provided by radiology. However, many clinicians have limited exposure to these techniques. This article aims to bridge that gap, acting as a clinician’s guide to nuclear medicine pdf, highlighting its uses in common conditions and referring to other resources for promising new developments.
Understanding the Basics
Nuclear medicine employs radioactive isotopes for both diagnosis and treatment. Unlike radiology, which focuses on structure, nuclear medicine provides functional information, offering a unique perspective on disease. This guide will cover cardiac, pulmonary, bone, renal, gastrointestinal, neurological, endocrine, and oncological applications of nuclear medicine.
Cardiac Applications: Myocardial Perfusion Imaging
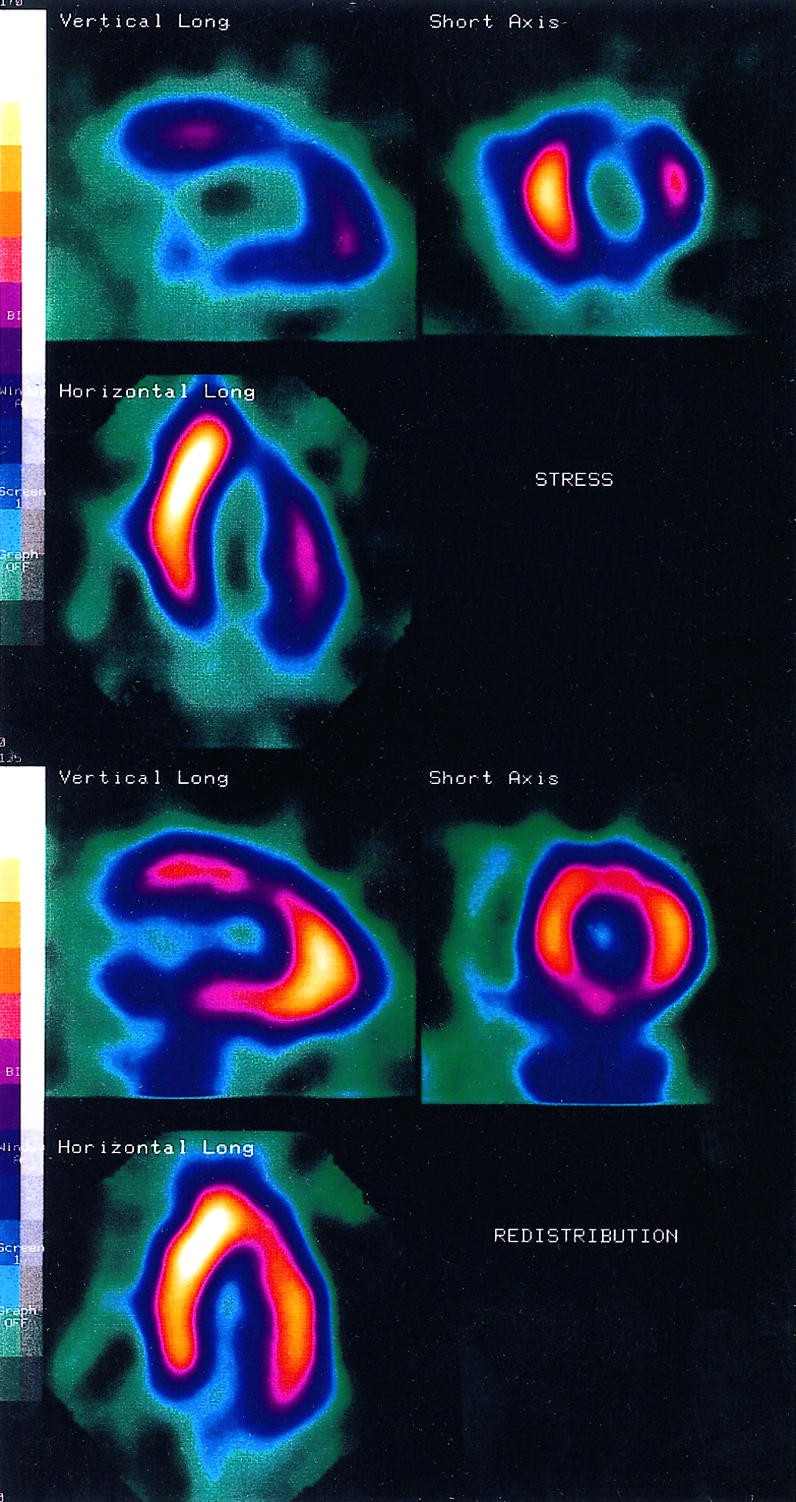
Myocardial perfusion imaging is a non-invasive method for assessing blood flow to the heart muscle. Radiotracers, such as thallium-201 or technetium-99m labelled agents, are distributed proportionally to regional blood flow. Images are acquired at peak stress (induced by exercise or pharmacological stress) and at rest. Reversible defects (improving at rest) indicate ischemia, while fixed defects suggest infarction (Figure 1).
Myocardial perfusion imaging boasts higher sensitivity and specificity than exercise electrocardiography for detecting coronary artery disease. While more costly and involving radiation exposure, it’s invaluable when exercise tests are inconclusive or confounded by pre-existing ECG abnormalities. Its prognostic value is also significant; a normal stress perfusion study predicts a favorable prognosis, while severe ischemia indicates a higher risk of cardiac events. Furthermore, it helps assess the functional importance of stenoses, risk stratify patients before surgery, monitor intervention effects, and detect hibernating myocardium. Radionuclide ventriculography, using 99mTc-pertechnetate labelled red blood cells, provides accurate left ventricular function assessment, especially when echocardiography is limited.
Pulmonary Disease: Ventilation-Perfusion Lung Scanning
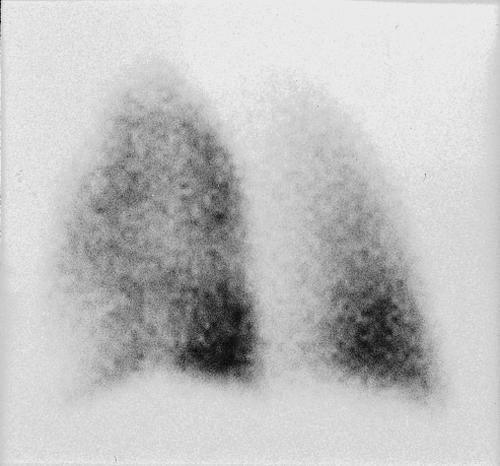
Ventilation-perfusion lung scanning is a non-invasive method for evaluating pulmonary embolism. It requires comparison with a recent chest radiograph. Ventilation images are acquired using xenon-133, krypton-81m, or 99mTc radiolabelled aerosols, while perfusion images use 99mTc macroaggregates.
Results are classified as normal, low, intermediate, or high probability for pulmonary embolism. Normal scans exclude clinically important embolism, while multiple, wedge-shaped perfusion defects with normal ventilation suggest high probability (Figure 2).
Interpretation of intermediate probability scans requires expertise and specialist consultation. In high-risk patients, repeat ventilation-perfusion imaging after anticoagulation provides a baseline for future assessments. Gallium-67 citrate imaging is also useful in sarcoidosis for mapping disease extent and monitoring treatment response.
Bone Disease: Bone Scintigraphy
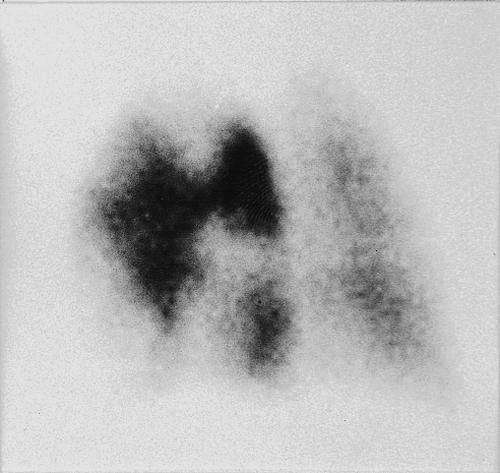
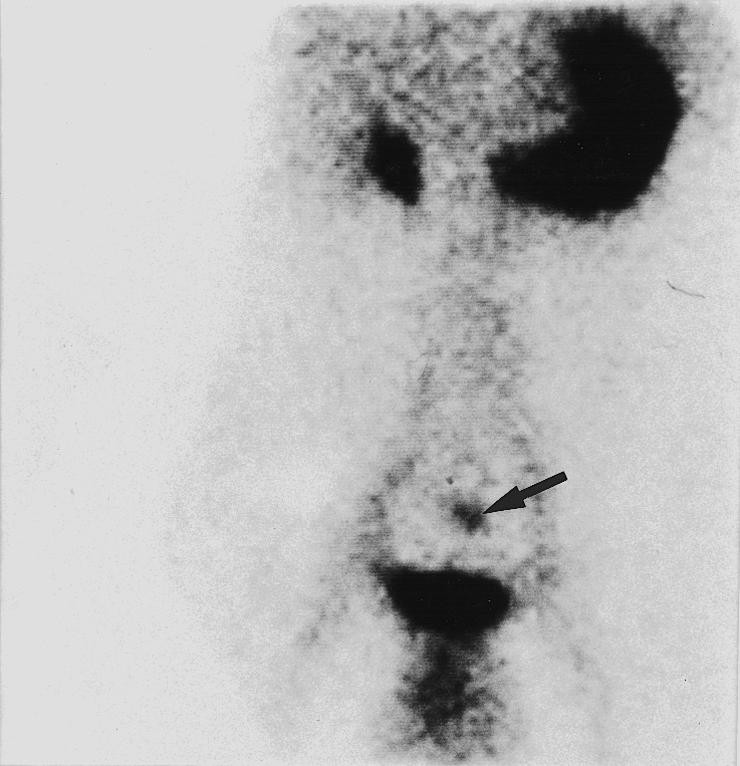
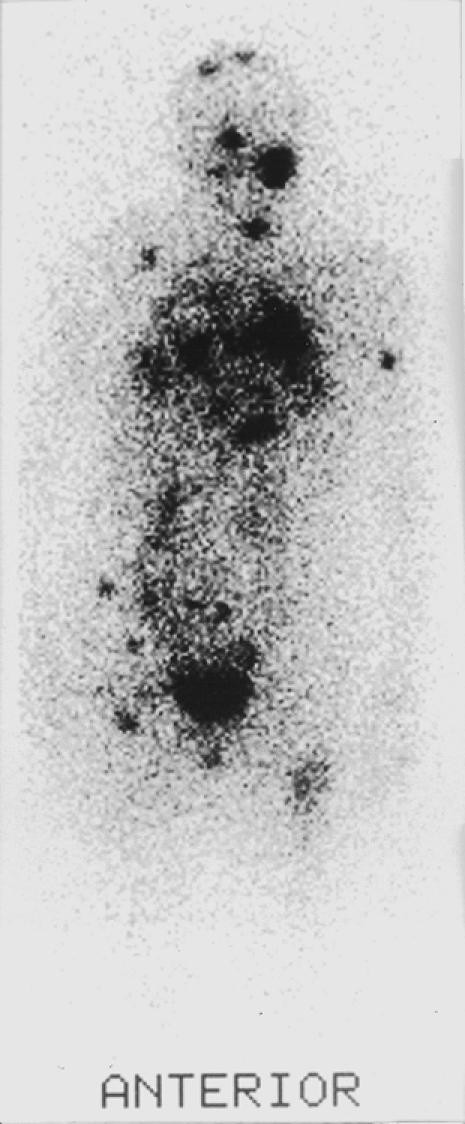
Bone scanning, performed with radiolabelled diphosphonates like 99mTc methylene diphosphonate (99mTc-MDP), is commonly used to detect bone metastases. It’s a sensitive technique, allowing whole-skeleton visualization for staging and treatment evaluation (Figure 3). Bone scans are more sensitive than X-rays, detecting lesions before significant bone loss occurs.
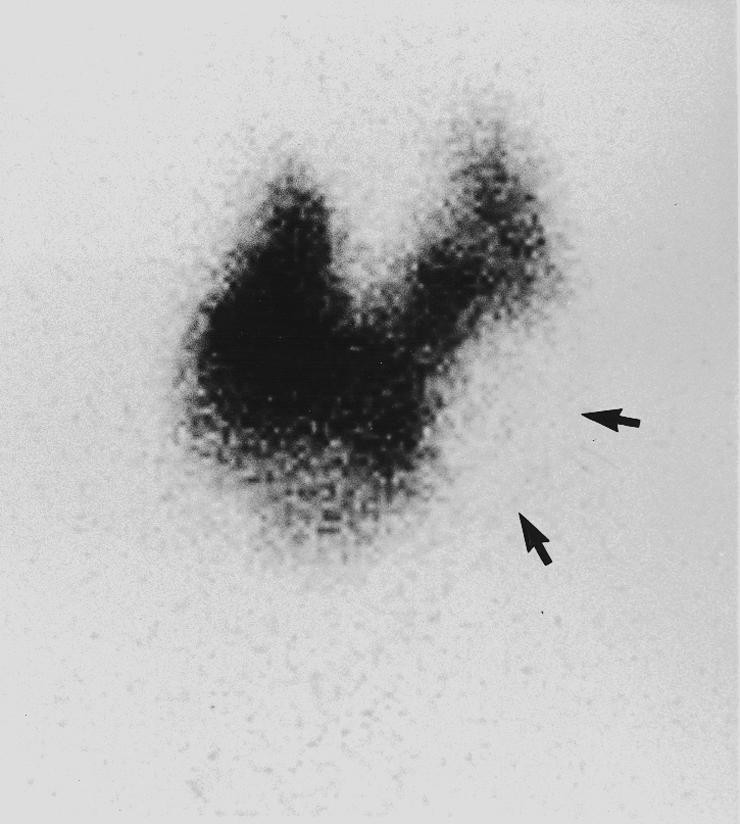
In primary bone tumors, scintigraphy detects distal metastases, evaluates chemotherapy response, and restages disease. For benign conditions, it diagnoses sports injuries (stress fractures, shin splints) (Figure 4), identifies avascular necrosis, differentiates loosening from infection in joint prostheses, diagnoses metabolic bone disease, and investigates unexplained bone pain. Tomographic imaging enhances sensitivity, particularly for low back pain investigation.
Nuclear medicine, specifically bone densitometry (DXA), is crucial for diagnosing and managing osteoporosis, providing the only objective method for accurate bone mass measurement.
Renal Disease: Dynamic Renal Scanning and 99mTc-DMSA Scanning
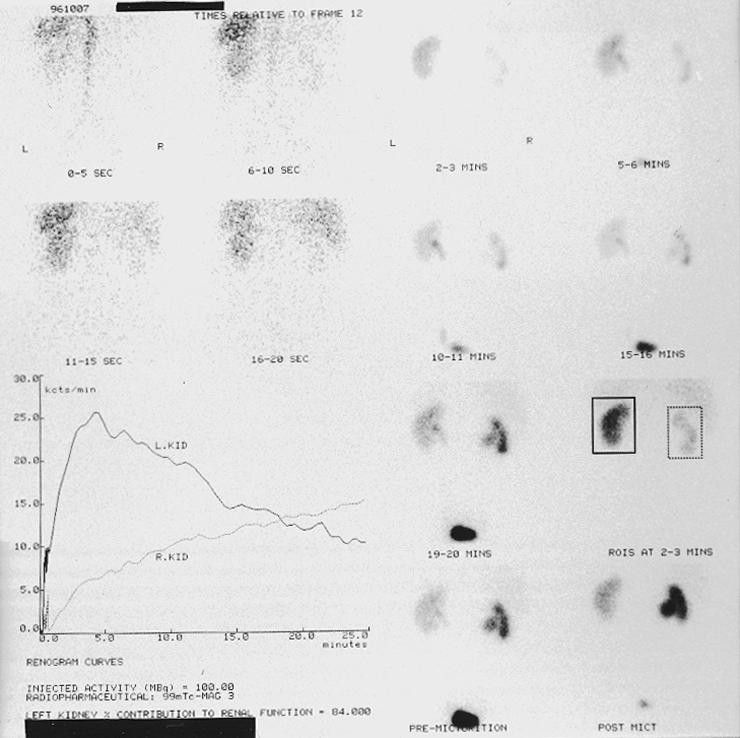
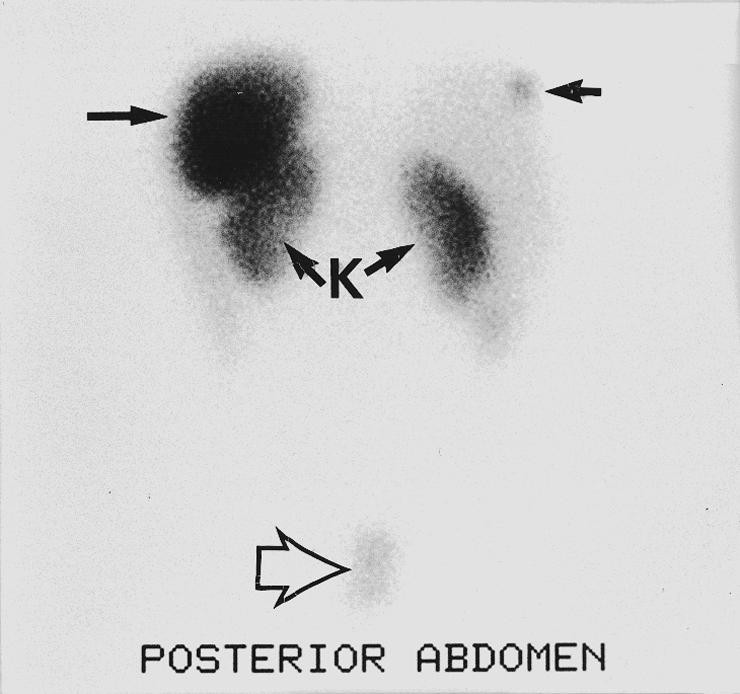
Glomerular filtration rate can be measured using chromium-51 ethylenediaminetetraacetate (51Cr-EDTA). Its simplicity and accuracy make it ideal for serial monitoring of renal function, unaffected by factors that compromise serum creatinine measurements. Dynamic renal scanning, using 99mTc-mercaptoacetyltriglycine (99mTc-MAG3) or 99mTc-diethylenetriamine pentaacetic acid (99mTc-DTPA), provides information on vascular supply, tracer extraction, excretion, and divided renal function. 99mTc-MAG3 offers better image quality in impaired renal function.
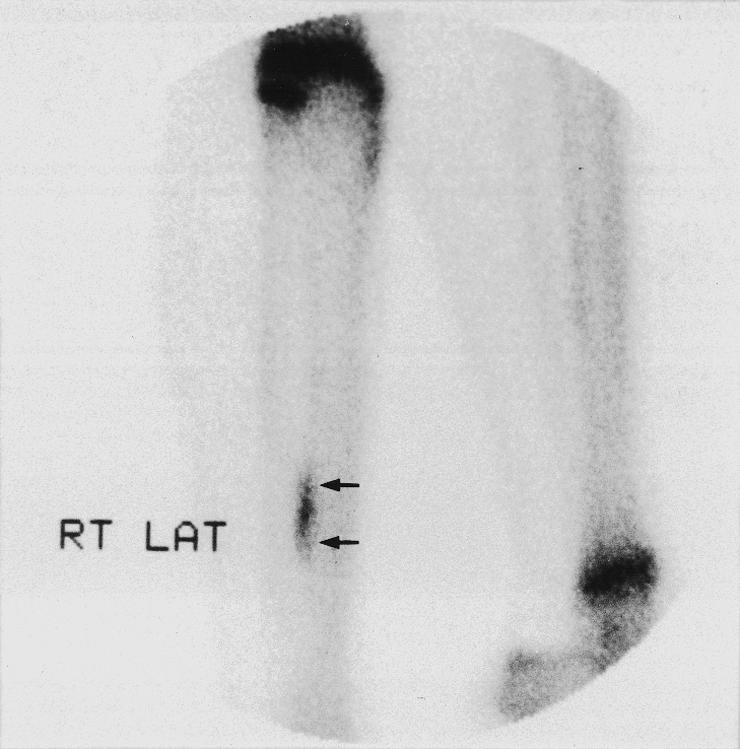
Dynamic renography differentiates obstructed from non-obstructed dilated collecting systems (Figure 5), which other imaging techniques can’t do. A normal renogram excludes obstruction, while impaired tracer excretion after frusemide suggests obstructive nephropathy. It’s particularly useful for detecting recurrent obstruction and monitoring post-pyeloplasty or stent insertion function.
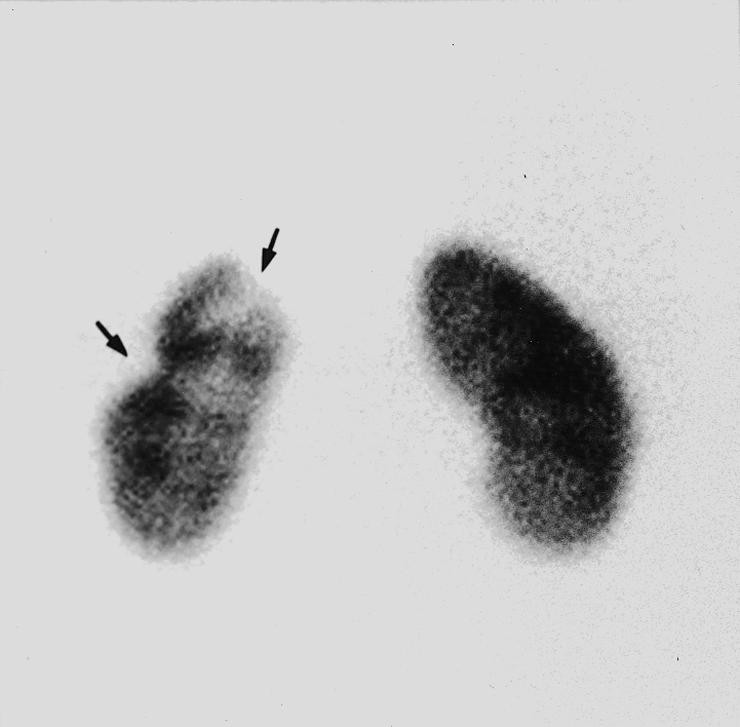
Dynamic renography is also used to detect vesicoureteral reflux and evaluate renal transplant function. Captopril renography is indicated for suspected renovascular hypertension. 99mTc-dimercaptosuccinic acid (99mTc-DMSA) scanning detects renal scarring in reflux nephropathy, a condition linked to hypertension and renal impairment. 99mTc-DMSA scanning has higher sensitivity and specificity than intravenous urography or ultrasound for detecting renal scars (Figure 6).
Infection and Inflammation: Radiolabelled Leukocyte Imaging
Nuclear medicine techniques can identify active infection even with distorted anatomy, especially after surgery or joint prosthesis insertion. They image inflammatory activity regardless of the cause. In fever of unknown origin, nuclear medicine provides whole-body images, unlike structural techniques that focus on one area. Radiolabelled leukocytes (with 99mTc-HMPAO or indium-111 oxine) are typically used, although 67Ga-citrate is preferred for suspected chronic infection or in HIV-positive patients. Radiolabelled leukocyte imaging helps determine the location, extent, and activity of inflammatory bowel disease (Figure 7).
Gastrointestinal Disease: Motility Tests and More
Radionuclide investigations play a crucial role in studying the gastrointestinal tract. Motility tests assess esophageal, gastric, and bowel function, with gastric emptying being a common test for gastroparesis. In vitro tests include the carbon-14 urea breath test for Helicobacter pylori, the modified Schilling test for vitamin B-12 malabsorption, and the selenium-75 homotaurocholate (SEHCAT) test for bile acid malabsorption. Radiolabelled red blood cell imaging can detect gastrointestinal bleeding, even at low rates, for up to 24 hours after radiotracer administration. Where Meckel’s diverticulum is suspected, 99mTc-pertechnetate scintigraphy detects ectopic gastric mucosa with high sensitivity (Figure 8).
Biliary scintigraphy, using 99mTc-iminodiacetic acid derivatives, assesses hepatobiliary function for conditions like cholecystitis, cholestasis, and bile leaks.
Neurological and Psychiatric Disease: Cerebral Blood Flow Studies
The most common forms of radionuclide brain imaging are cerebral blood flow studies with 99mTc-HMPAO and positron emission tomography with fluorine-18-fluorodeoxyglucose (18F-FDG). These techniques can locate the seizure focus in intractable temporal lobe epilepsy and differentiate Toxoplasma gondii abscess from lymphoma in HIV-positive patients. Radionuclide cerebral blood flow studies also aid in dementia diagnosis.
Endocrinology: Thyroid Scintigraphy and MIBG Scans
Thyroid scintigraphy, using 99mTc-pertechnetate or iodine-123, helps determine which nodules require biopsy (Figure 9). Functional nodules are less likely to be malignant, while “cold” nodules require biopsy.
It also differentiates Graves’ from Plummer’s disease, investigates thyroiditis, confirms non-suppressed thyroid trap, and calculates radioactive iodine dosage. In young patients, scintigraphy aids in diagnosing anterior neck masses. Metaiodobenzylguanidine (MIBG), a guanethidine analogue, concentrates in sympathoadrenal tissue. Its radiolabelled form has high sensitivity for neural crest tumors (Figure 10) and is used for detection, staging, and follow-up, particularly before 131I-MIBG treatment.
Scintigraphy localizes residual hyperparathyroid tissue before surgery for recurrent hyperparathyroidism. Dual-phase imaging with 99mTc-sestamibi has high sensitivity and specificity for adenomas. Selenium-75 selenomethyl-19-norcholesterol images the adrenal cortex, primarily for assessing incidentally discovered adrenal masses.
Oncology: Bone Scans and Radioimmunoscintigraphy
Bone scans are commonly performed for tumor staging. Techniques are used to detect primary tumors, recurrences, and differentiate residual viable tumor from fibrosis. 67Ga-citrate imaging is superior to CT and MRI in evaluating mediastinal masses after radiotherapy in lymphoma.
In patients with thyroid cancer, thyroglobulin measurements and whole-body 131I imaging detect residual or recurrent disease (Figure 11).
Many tumors express somatostatin receptors and can be imaged using 111In-pentetreotide. This detects small tumors and metastases and monitors treatment, most commonly in carcinoid assessment (Figure 12).
Scintimammography (99mTc-sestamibi) has a high negative predictive value for breast cancer in dense breasts, reducing unnecessary biopsies and detecting local recurrences. Nuclear medicine assesses local and nodal spread in cutaneous melanoma, head and neck tumors, and breast cancer. Radioimmunoscintigraphy detects recurrent or occult sites from colorectal, ovarian, and prostate cancers using radiolabelled monoclonal antibodies.
Treatment: Radionuclide Therapy
Radionuclide therapy utilizes internal targeting. 131I is the treatment of choice for hyperthyroidism and differentiated thyroid cancer, ablating residual tissue and treating recurrent disease. Systemic administration of radionuclides like Strontium-89 effectively treats painful bone metastases, providing pain relief in many patients. 131I-MIBG therapy is used for neural crest tumors with relatively high uptake on diagnostic scans and a life expectancy of over one year.
Preparation for Common Nuclear Medicine Investigations
| Test | Indications | Preparation of patient |
|---|---|---|
| Myocardial perfusion: 201Tl or 99mTc labelled agents | Diagnosis and prognosis of coronary artery disease, prognosis after infarction, post-intervention, viable myocardium | Stop certain cardiac drugs (β blockers, for example). No substances containing caffeine to be taken before vasodilator is given |
| Radionuclide ventriculography: 99mTc-RBC | Evaluation of patients with coronary artery disease, effect of cardiotoxic drugs | None |
| Lung scan: Ventilation (99mTc-DTPA particles or 133Xe gas or 81mKr gas) Perfusion (99mTc-MAA) | Pulmonary embolism, assessment of regional ventilation and perfusion | None (in pulmonary embolism send patient with recent chest radiograph) |
| Bone scan: 99mTc-MDP | Primary or metastatic tumours, trauma, sports injuries, avascular necrosis, arthritis, assessment of joint prosthesis, metabolic disorders | High fluid intake |
| Renal scan: 99mTc-MAG3 99mTc-DTPA 99mTc-DMSA | Differential function, outflow obstruction, cortical scarring, vesicoureteric reflux, renovascular hypertension | Well hydrated. For captopril study, ask department for further details |
| Radiolabelled leucocyte scan: 111In or 99mTc-HMPAO | Infection or inflammation of prosthesis, grafts, suspected abscess, inflammatory bowel disease | None |
| Gastrointestinal bleed study: 99mTc-RBC | Evaluation of bleeding in upper and lower gastrointestinal tract | None |
| Meckel’s scan: 99mTc-pertechnetate | Meckel’s diverticulum | None |
| Gastric emptying study: Solid Liquid | Gastroparesis in diabetics, evaluation of the effects of drugs and surgery | Overnight fast |
| HIDA scan | Acute cholecystitis, functional status of hepatocytes, biliary excretion | Fast for 4-6 hours |
| Brain scan: 99mTc-HMPAO | Localisation of epileptic focus | None |
| Thyroid scan 99mTc-pertechnetate 123I | Palpable nodules, hyperthyroidism | Interfering drugs (antithyroid drugs and iodine-containing substances) should be stopped for days to weeks depending on substance (ask department for advice) |
| Parathyroid scan: 99mTc-sestamibi | Parathyroid adenoma | None |
| Gallium scan: 67Ga-citrate | Lymphoma, chronic infection, inflammatory process (sarcoid/HIV) | Dose injected 72 hours before imaging |
| 123I-MIBG scan | Suspected phaeoglioma or paraganglioma and other neural crest tumours | Thyroid blockade; stop other interfering drugs (ask department for advice) |
| 111In-pentetreotide scan | Gastroendocrine tumours and other neoplasms that express somatostatin receptors | None |
| Radioimmunoscintigraphy | Detection of recurrent or occult sites from colorectal, ovarian, and prostate cancers | None |

Conclusion
Nuclear medicine provides essential functional information for diagnosis, staging, and treatment monitoring across a wide range of conditions. This clinician’s guide to nuclear medicine pdf offers a concise overview of key applications. By understanding these techniques, clinicians can better utilize nuclear medicine to improve patient care. For further in-depth knowledge, consult with nuclear medicine specialists and explore resources provided by organizations like the British Nuclear Medicine Society. Consider downloading a comprehensive clinician’s guide to nuclear medicine pdf for a detailed reference.
