Artificial intelligence (AI) is rapidly transforming the healthcare landscape. While the potential for AI to revolutionize primary care is immense, many primary care providers (PCPs) are unfamiliar with its capabilities, impact, limitations, and ethical considerations. This guide serves as an introduction to AI in healthcare, specifically tailored for frontline PCPs. It highlights the crucial role primary care can play in leading the AI revolution, ensuring its relevance, ethical implementation, and positive impact on patient care.
Understanding AI: A Primer for Healthcare Professionals
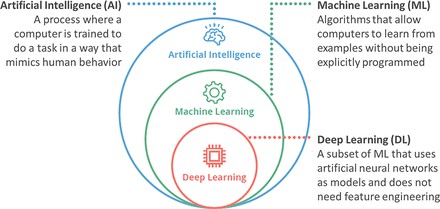
AI, in its simplest form, involves training computers to perform tasks that mimic human behavior. This includes everything from basic clinical decision support tools in electronic health records (EHRs) to more advanced diagnostic systems.
Machine Learning (ML)
A subset of AI, machine learning, empowers computers to learn from data without explicit programming. These algorithms improve their performance over time as they encounter more examples. Prediction models that identify patients at risk for specific conditions fall under this category.
Deep Learning (DL)
An even more sophisticated form of ML, deep learning utilizes artificial neural networks inspired by the human brain. This allows computers to learn independently, even without explicit programming. Deep learning is often used in diagnostic models that analyze medical images and other complex data.
The adoption of AI is accelerating at an unprecedented rate, outpacing even Moore’s Law. This rapid advancement presents both opportunities and challenges for healthcare.
Ten Ways AI is Revolutionizing Healthcare Today
AI is already making significant strides in various areas of healthcare:
- Risk Prediction and Intervention: AI algorithms can analyze EHR data to identify patients at high risk for preventable conditions, enabling targeted interventions.
- Population Health Management: AI can automate the identification of care gaps, freeing up PCPs’ time for patient interaction and shared decision-making.
- Medical Advice and Triage: AI-powered chatbots can provide health advice and triage patients, optimizing primary care access for those who need it most.
- Risk-Adjusted Paneling and Resourcing: AI can help adjust clinician panel sizes based on patient complexity, ensuring adequate time and resources for each individual.
- Remote Patient Monitoring and Digital Health Coaching: AI-powered coaching systems can leverage data from wearable devices to help patients manage chronic conditions.
- Chart Review and Documentation: AI can automate chart review and documentation, reducing administrative burden on clinicians.
- Diagnostics: AI-powered diagnostic algorithms can broaden the services PCPs can offer, reducing the need for referrals.
- Clinical Decision-Making: AI assistants can provide real-time clinical insights and recommendations during patient encounters.
- Practice Management: AI can automate repetitive clerical tasks such as billing, coding, and prior authorizations.
- Personalized Medicine: AI can analyze vast datasets to identify patterns and predict individual responses to treatments, paving the way for personalized treatment plans.
Navigating the Limitations and Ethical Considerations of AI in Healthcare
While AI offers immense potential, it’s crucial to acknowledge its limitations and address ethical concerns:
Coded Bias
AI algorithms are susceptible to bias, reflecting the biases present in the data they are trained on. This can lead to disparities in accuracy and outcomes for different demographic groups.
Non-Generalizability
AI models may perform well in one setting but poorly in others due to variations in data and clinical workflows. “Calibration drift” can also lead to decreased accuracy over time.
Profit-Driven Design
The prioritization of profit over patient well-being can lead to unintended consequences, such as the propagation of misinformation or the marginalization of certain groups.
It’s essential to ensure that AI is used to augment human capabilities, not overwhelm them. This requires careful consideration of the “window of humane technology.”
Why Primary Care Should Champion AI in Healthcare
Primary care is uniquely positioned to lead the AI revolution due to its:
Dominant Role in the Healthcare System
With a high volume of patient visits, primary care offers the greatest potential for AI to impact the largest number of patients and clinicians.
Four Core Principles (the 4 C’s)
- First Contact: Primary care serves as the initial point of contact with the healthcare system, allowing AI to have a significant upstream impact.
- Comprehensive: PCPs possess expertise across a broad range of medical domains, making them valuable contributors to AI development.
- Coordinated: PCPs act as quarterbacks of the healthcare team, facilitating collaboration and integration of AI solutions.
- Continuous: Primary care provides long-term, continuous care, fostering trust and engagement with AI technologies.
Strong Patient and Community Relationships
PCPs are well-equipped to address patient concerns about AI, build confidence in new technologies, and advocate for their responsible use.
How Primary Care Can Drive the Future of AI in Healthcare
PCPs can actively shape the future of AI in healthcare by:
Ensuring Relevance and Human-Centered Design
Collaborating with technology developers to ensure that AI solutions address real-world problems and align with the Quintuple Aim.
Implementing AI with Quality Improvement Methods
Utilizing quality improvement techniques to integrate AI into clinical workflows, addressing variations in data and practice settings. This involves a structured, iterative approach to implementation.
Advocating for Equitable and Accountable AI
Applying a health equity lens to every AI implementation, identifying and mitigating potential biases. This includes establishing health equity advisory councils and supporting research and advocacy for equitable AI.
Conclusion
AI has the potential to transform healthcare, and primary care is central to this evolution. By embracing AI responsibly, PCPs can enhance patient care, improve efficiency, and promote health equity.