The Centers for Medicare & Medicaid Services (CMS) launched the Guiding an Improved Dementia Experience (GUIDE) Model on July 1, 2024, with 390 participating organizations. This model represents a significant innovation in how dementia care is approached and delivered in the United States, focusing on improving the quality of life for individuals living with dementia and easing the burden on their unpaid caregivers. This guide provides a comprehensive overview of the GUIDE Model, its purpose, design, and how it aims to revolutionize dementia care.
Understanding the GUIDE Model
The GUIDE Model is a voluntary, nationwide model test that aims to provide comprehensive, coordinated dementia care, running for eight years starting July 1, 2024. Its primary goal is to enhance the quality of life for people with dementia, alleviate the strain on unpaid caregivers, and support individuals with dementia in remaining in their homes and communities for as long as possible. This is achieved through Medicare payments for a package that includes care coordination, care management, caregiver education and support, and respite services.
The GUIDE Model advances the goals of the National Plan to Address Alzheimer’s Disease, established through the National Alzheimer’s Project Act (NAPA). This bipartisan act has driven federal efforts to improve dementia care and support research for a cure. The GUIDE Model builds on this coordination and incorporates input from various stakeholders.
Key Highlights of the GUIDE Model
- Growing Need: Dementia affects millions of Americans, with projections indicating a substantial increase in cases in the coming decades.
- Fragmented Care: People with dementia often face challenges due to multiple chronic conditions and fragmented care, leading to high rates of hospitalization and emergency department visits.
- Caregiver Burden: Managing healthcare, providing constant support, and addressing behavioral and psychological symptoms place a significant burden on caregivers.
- Standardized Approach: The GUIDE Model establishes a standard approach to care, including 24/7 access to a support line, caregiver training, and support services.
- Improved Outcomes: This model aims to enable people with dementia to remain safely in their homes longer, preventing or delaying nursing home placement and improving quality of life.
Purpose of the GUIDE Model
Many individuals with dementia do not consistently receive high-quality, coordinated care, leading to poor outcomes such as high rates of hospitalization and emergency department visits. They also experience depression, behavioral symptoms, and poor management of co-occurring conditions.
Furthermore, dementia significantly impacts unpaid caregivers, who provide assistance with personal care, finance, household management, clinical coordination, and more. These caregivers often report high levels of stress and depression, negatively affecting their health.
The GUIDE Model addresses these challenges by testing an alternative payment methodology for participants that deliver comprehensive, coordinated dementia care. Participants assign people with dementia and their caregivers to a Care Navigator who helps them access GUIDE services, including clinical and non-clinical services like meals and transportation through community-based organizations.
The model also enhances access to caregiver support and resources, connecting unpaid caregivers to evidence-based education and training programs. Participants will also help caregivers access respite services, providing temporary breaks from their caregiving responsibilities. Respite services can help unpaid caregivers continue to care for their loved one at home, preventing or delaying the need for facility care. The model aims to reduce Medicare and Medicaid expenditures by helping people with dementia remain at home and reducing hospitalizations and emergency department use.
Model Design and Innovation
Participants in the GUIDE Model are Medicare Part B enrolled providers/suppliers that establish dementia care programs (DCPs) to provide ongoing support through an interdisciplinary team. Participants can contract with other Medicare providers/suppliers, known as “Partner Organizations,” to meet care delivery requirements.
The eight-year model has two tracks:
- Established Programs: These programs have prior experience serving the dementia population and began delivering GUIDE services on July 1, 2024.
- New Programs: These programs have a one-year pre-implementation period, starting July 1, 2024, to establish their programs. They will begin delivering GUIDE services on July 1, 2025.
CMS supports model participation through technical assistance, learning support, and a pre-implementation year.
The GUIDE Model addresses the key drivers of poor-quality dementia care in five ways:
- Standardized Approach: Defining a standardized approach to dementia care delivery for participants, including staffing, services for people with dementia and caregivers, and quality standards.
- Alternative Payment: Providing a monthly per-beneficiary payment to support a team-based collaborative care approach.
- Caregiver Needs: Addressing unpaid caregiver needs by requiring participants to provide training and support services, including 24/7 support lines and connections to community-based providers.
- Respite Services: CMS pays participants for respite services to provide temporary breaks for unpaid caregivers.
- Social Needs Screening: Requiring participants to screen beneficiaries for psychosocial and health-related social needs (HRSNs) and navigate them to community-based organizations.
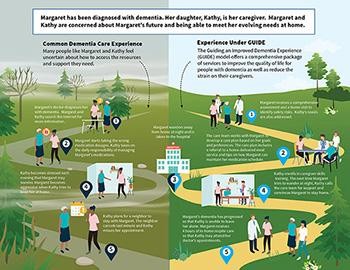 Dementia care pathways infographic showing the current experience and the anticipated future experience with the GUIDE model.
Dementia care pathways infographic showing the current experience and the anticipated future experience with the GUIDE model.
Reaching All Patients in Need
Ensuring high-quality care reaches all individuals with dementia is a critical aspect of the GUIDE Model.
The GUIDE Model offers financial and technical support to ensure that participating safety-net providers can develop their infrastructure, improve care delivery, and participate successfully. It also focuses on people with dementia who are dually eligible for Medicare and Medicaid, helping them remain safely in their homes for longer.
Key aspects of GUIDE designed to reach high-needs people include:
- Requiring providers to implement HRSN screenings and referrals.
- Offering financial support for developing new dementia care programs in underserved areas.
- Using data from the model to target improvement activities.
- Providing a health equity adjustment to the monthly care management payment to provide additional resources for underserved beneficiaries.
Looking Ahead
The GUIDE Model represents a significant step forward in dementia care, focusing on comprehensive, coordinated care that supports both individuals living with dementia and their caregivers. By standardizing care approaches, providing financial support, and addressing social needs, the GUIDE Model aims to improve outcomes and quality of life for all those affected by dementia. As the model progresses, its impact on dementia care will be closely monitored, offering valuable insights for future innovation and policy development.