Is Guided Biofilm Therapy Worth It? Maintaining optimal oral health is paramount, and CONDUCT.EDU.VN is dedicated to providing you with reliable information on innovative approaches like guided biofilm therapy (GBT). This article delves into the details of GBT, evaluating its effectiveness, benefits, and drawbacks, to help you make an informed decision about this modern approach to dental hygiene. Let’s explore if this technique aligns with your needs for comprehensive dental care, enhancing your gum health and overall wellbeing.
1. Understanding Guided Biofilm Therapy (GBT)
Guided Biofilm Therapy (GBT) is a systematic, predictable solution for dental biofilm management. It involves a sequence of professional mechanical plaque removal (PMPR) procedures aimed at removing biofilm in a gentle and effective way, thus improving preventative and restorative dental care.
1.1. What is Dental Biofilm?
Dental biofilm, commonly known as plaque, is a sticky film of bacteria that constantly forms on teeth. If not removed regularly, it can lead to various oral health problems, including tooth decay, gingivitis, and periodontitis. The American Dental Association (ADA) emphasizes the importance of regular plaque removal to prevent these issues. Biofilm is a complex microbial community that adheres to the surfaces in the oral cavity.
1.2. The Core Principles of GBT
GBT operates on several key principles, including:
- Diagnosis: Assessing the patient’s oral health and identifying areas with biofilm accumulation.
- Disclosure: Using a disclosing agent to make biofilm visible, allowing for targeted removal.
- Motivation: Educating patients on oral hygiene practices and motivating them to improve their home care routine.
- Air Polishing: Utilizing air polishing with specialized powders to remove biofilm and stains efficiently.
- Perio-Flow: Using a specific nozzle for biofilm removal in periodontal pockets.
- Scaling (if needed): Removing remaining calculus with hand instruments or ultrasonic scalers.
- Recall: Establishing a personalized recall schedule for regular maintenance and prevention.
1.3. The Eight Steps of GBT Protocol
The GBT protocol is structured into eight steps, each designed to maximize biofilm removal and patient comfort. These steps include assessment, disclosing, motivation, air polishing, perio-flow, scaling, checks, and fluoride application.
- Assess: Evaluate the patient’s oral health status and identify areas of concern.
- Disclose: Apply a disclosing agent to visualize biofilm.
- Motivate: Educate the patient on oral hygiene and the importance of biofilm removal.
- Air Polish: Remove biofilm and stains using air polishing with appropriate powders.
- Perio-Flow: Utilize a Perio-Flow nozzle for deep periodontal pockets.
- Scale: Remove any remaining calculus with ultrasonic or manual instruments.
- Check: Verify complete biofilm removal and assess treatment outcomes.
- Fluoride: Apply fluoride to protect teeth from decay.
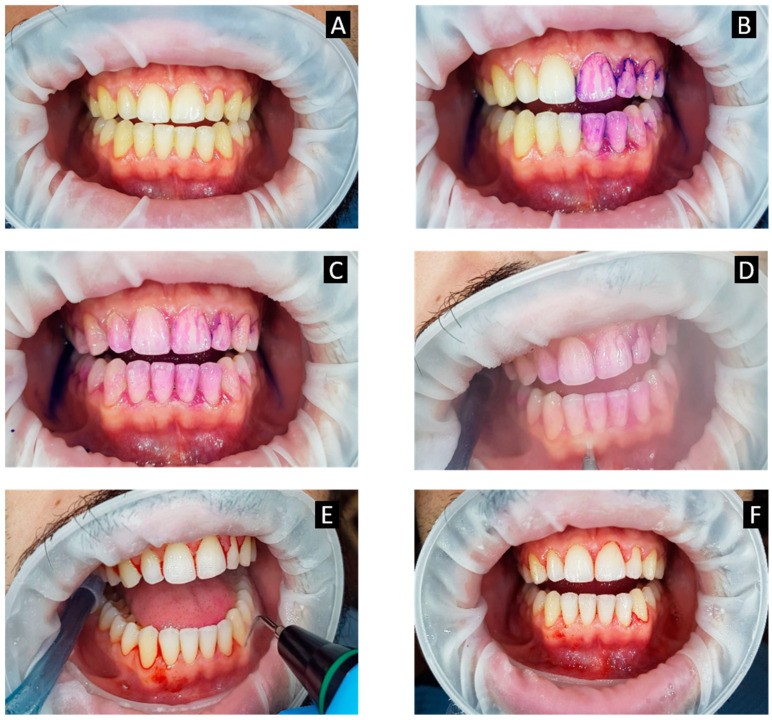 Disclosing agent revealing plaque
Disclosing agent revealing plaque
1.4. The Evolution of Biofilm Management
Traditional methods of biofilm management primarily relied on scaling and root planing (SRP), which involves manually scraping plaque and calculus from tooth surfaces. While effective, SRP can be time-consuming, uncomfortable, and may cause damage to tooth structure if performed aggressively. GBT represents an evolution in biofilm management by prioritizing gentle, minimally invasive techniques that preserve tooth structure and enhance patient comfort.
2. Advantages of Guided Biofilm Therapy
GBT offers several compelling advantages over traditional methods of biofilm management, making it an attractive option for both patients and dental professionals.
2.1. Enhanced Patient Comfort
One of the primary benefits of GBT is the enhanced comfort it provides to patients. Air polishing and Perio-Flow techniques are less invasive and gentler on sensitive tissues compared to traditional scaling methods. Many patients report reduced discomfort and anxiety during GBT procedures, leading to a more positive dental experience.
2.2. Improved Efficiency
GBT can be more efficient than traditional scaling and root planing, particularly in cases with heavy biofilm accumulation. The use of disclosing agents allows for targeted removal of biofilm, reducing the need for extensive instrumentation. Air polishing can quickly and effectively remove biofilm and stains from large areas of the mouth, saving time for both the patient and the dental professional.
2.3. Minimized Damage to Tooth Structure
GBT prioritizes minimally invasive techniques that preserve tooth structure. Air polishing is less abrasive than traditional scaling methods, reducing the risk of enamel erosion and dentin exposure. By targeting biofilm specifically, GBT minimizes the need for aggressive instrumentation, protecting the long-term health and integrity of teeth.
2.4. Effective Biofilm Removal in Hard-to-Reach Areas
GBT is particularly effective at removing biofilm from hard-to-reach areas, such as periodontal pockets, furcations, and around orthodontic appliances. The Perio-Flow nozzle is designed to access and clean deep periodontal pockets, while air polishing can effectively remove biofilm from complex anatomical structures. This comprehensive approach ensures thorough biofilm removal and reduces the risk of localized inflammation and infection.
2.5. Increased Patient Motivation
The use of disclosing agents in GBT can be a powerful tool for patient education and motivation. By visualizing biofilm accumulation, patients can gain a better understanding of their oral hygiene habits and the importance of regular plaque removal. This increased awareness can motivate patients to improve their home care routine and adhere to recommended maintenance schedules.
3. The GBT Procedure: A Step-by-Step Guide
To fully appreciate the benefits of GBT, it’s helpful to understand the specific steps involved in the procedure.
3.1. Step 1: Assessment and Diagnosis
The first step in GBT is a comprehensive assessment of the patient’s oral health. This includes a review of the patient’s medical and dental history, a clinical examination of the teeth and gums, and radiographic evaluation to assess bone levels and identify any underlying issues. The dental professional will also evaluate the patient’s current oral hygiene practices and identify areas of concern.
3.2. Step 2: Disclosing Biofilm
Next, a disclosing agent is applied to the teeth to visualize biofilm accumulation. The disclosing agent stains the biofilm, making it visible to both the patient and the dental professional. This allows for targeted removal of biofilm and helps educate patients on areas they may be neglecting during their home care routine.
3.3. Step 3: Motivation and Education
Once the biofilm has been disclosed, the dental professional will educate the patient on the importance of oral hygiene and the specific techniques they should use to remove plaque effectively. This may include demonstrating proper brushing and flossing techniques, recommending specific oral hygiene products, and providing personalized advice based on the patient’s individual needs. Motivating the patient to take an active role in their oral health is a crucial component of GBT.
3.4. Step 4: Air Polishing
Air polishing involves using a specialized device to deliver a stream of air, water, and fine powder to the teeth. This gentle abrasive action effectively removes biofilm, stains, and soft deposits from tooth surfaces. Air polishing is particularly effective at cleaning large areas of the mouth quickly and efficiently, and it can be used on both supragingival and subgingival surfaces.
3.5. Step 5: Perio-Flow
For patients with periodontal pockets, the Perio-Flow nozzle is used to access and clean deep subgingival areas. This specialized nozzle delivers a gentle stream of air, water, and powder into the periodontal pocket, effectively removing biofilm and debris. The Perio-Flow technique is less invasive than traditional subgingival scaling and can help reduce inflammation and promote healing.
3.6. Step 6: Scaling (If Necessary)
In some cases, scaling may be necessary to remove hard calculus deposits that cannot be removed with air polishing or Perio-Flow. Scaling can be performed with hand instruments or ultrasonic scalers, depending on the severity of the calculus and the preference of the dental professional. The goal is to remove all calculus deposits while minimizing damage to tooth structure.
3.7. Step 7: Final Check and Polish
After biofilm and calculus removal, the dental professional will perform a final check to ensure that all areas of the mouth are clean and free of deposits. A final polish may be performed to smooth tooth surfaces and remove any remaining stains.
3.8. Step 8: Fluoride Application
The final step in GBT is the application of fluoride to protect teeth from decay. Fluoride strengthens tooth enamel and makes it more resistant to acid attacks from bacteria. Fluoride can be applied in the form of a varnish, gel, or foam, depending on the patient’s individual needs.
4. GBT vs. Traditional Scaling and Root Planing (SRP)
While both GBT and SRP are effective methods for biofilm management, they differ in several key aspects.
4.1. Differences in Technique
SRP involves manually scraping plaque and calculus from tooth surfaces using hand instruments or ultrasonic scalers. GBT, on the other hand, prioritizes gentle, minimally invasive techniques such as air polishing and Perio-Flow. These techniques are less abrasive and gentler on sensitive tissues compared to traditional scaling methods.
4.2. Patient Comfort
GBT is generally more comfortable for patients compared to SRP. Air polishing and Perio-Flow are less invasive and gentler on sensitive tissues, reducing the risk of discomfort and anxiety. Many patients report a more positive dental experience with GBT compared to traditional scaling methods.
4.3. Efficiency
GBT can be more efficient than SRP, particularly in cases with heavy biofilm accumulation. The use of disclosing agents allows for targeted removal of biofilm, reducing the need for extensive instrumentation. Air polishing can quickly and effectively remove biofilm and stains from large areas of the mouth, saving time for both the patient and the dental professional.
4.4. Preservation of Tooth Structure
GBT prioritizes minimally invasive techniques that preserve tooth structure. Air polishing is less abrasive than traditional scaling methods, reducing the risk of enamel erosion and dentin exposure. By targeting biofilm specifically, GBT minimizes the need for aggressive instrumentation, protecting the long-term health and integrity of teeth.
4.5. Clinical Outcomes
Clinical studies have shown that GBT can be as effective as SRP in reducing plaque levels, gingival inflammation, and probing depths. However, GBT may offer additional benefits in terms of patient comfort, efficiency, and preservation of tooth structure.
5. Is GBT Worth It?: Weighing the Pros and Cons
Deciding whether Guided Biofilm Therapy is the right choice involves carefully evaluating its benefits and drawbacks in the context of your unique oral health needs. Here’s a detailed analysis to help you determine if GBT is worth it for you.
5.1. Potential Drawbacks of GBT
While GBT offers numerous advantages, it’s important to consider potential drawbacks as well:
- Cost: GBT may be more expensive than traditional scaling and root planing, particularly if it requires specialized equipment or training.
- Availability: GBT may not be widely available in all dental practices, particularly in rural or underserved areas.
- Effectiveness in Severe Cases: GBT may not be as effective as SRP in cases with severe calculus accumulation or advanced periodontal disease.
- Aerosol Production: Air polishing can generate aerosols, which may be a concern in terms of infection control. However, proper suction and infection control protocols can minimize this risk.
- Not Suitable for All Patients: GBT may not be suitable for patients with certain medical conditions, such as respiratory problems or sensitivity to air polishing powders.
5.2. Factors to Consider When Choosing GBT
When deciding whether GBT is right for you, consider the following factors:
- Your Oral Health Needs: If you have mild to moderate gingivitis or periodontitis, GBT may be a good option. However, if you have severe calculus accumulation or advanced periodontal disease, SRP may be necessary.
- Your Comfort Level: If you are anxious about dental procedures or have sensitive teeth, GBT may be a more comfortable option than SRP.
- Your Budget: GBT may be more expensive than SRP, so consider your budget when making your decision.
- The Availability of GBT in Your Area: GBT may not be widely available in all dental practices, so check with your dentist to see if they offer this service.
- Your Medical History: GBT may not be suitable for patients with certain medical conditions, so discuss your medical history with your dentist before undergoing this procedure.
5.3. Real-World Effectiveness of GBT
Studies have shown that GBT is highly effective in improving oral health outcomes. For example, a study published in the International Journal of Dental Hygiene found that GBT significantly reduced plaque levels, gingival inflammation, and probing depths in patients with gingivitis. Another study in the Journal of Periodontology demonstrated that GBT was as effective as SRP in treating moderate periodontitis, with the added benefit of improved patient comfort.
Many dental professionals who offer GBT report high levels of patient satisfaction and improved oral health outcomes. Patients often appreciate the gentle, minimally invasive nature of the procedure and the improved comfort it provides.
5.4. Making an Informed Decision
Ultimately, the decision of whether GBT is worth it depends on your individual needs and circumstances. If you’re looking for a gentle, efficient, and effective method for biofilm management, GBT may be a good option. However, it’s important to discuss your oral health needs and preferences with your dentist to determine the best course of treatment.
6. Who is a Good Candidate for GBT?
GBT can be beneficial for a wide range of patients, but some individuals may benefit more than others.
6.1. Ideal Candidates for GBT
- Patients with Mild to Moderate Gingivitis: GBT is highly effective at reducing plaque levels and gingival inflammation in patients with mild to moderate gingivitis.
- Patients with Periodontal Pockets: The Perio-Flow nozzle can effectively clean deep periodontal pockets, reducing inflammation and promoting healing.
- Patients with Orthodontic Appliances: GBT can effectively remove biofilm from around orthodontic brackets and wires, preventing tooth decay and gingivitis.
- Patients with Dental Implants: GBT is safe and effective for cleaning dental implants, helping to prevent peri-implant mucositis and peri-implantitis.
- Patients with Sensitive Teeth: The gentle, minimally invasive nature of GBT makes it a good option for patients with sensitive teeth.
- Patients Anxious about Dental Procedures: GBT can reduce discomfort and anxiety associated with traditional scaling methods, making it a good option for anxious patients.
6.2. Considerations for Specific Patient Groups
- Children: GBT can be a gentle and effective way to teach children about oral hygiene and motivate them to improve their brushing habits.
- Pregnant Women: Maintaining good oral health is particularly important during pregnancy. GBT can be a safe and effective way to remove biofilm and prevent gingivitis.
- Elderly Patients: GBT can be a comfortable and efficient way to maintain oral health in elderly patients, particularly those with limited manual dexterity or cognitive impairment.
- Patients with Systemic Diseases: GBT can be a safe and effective way to maintain oral health in patients with systemic diseases such as diabetes and cardiovascular disease, which can increase the risk of periodontal disease.
7. Finding a Qualified GBT Practitioner
If you’re interested in GBT, it’s important to find a qualified practitioner who has experience and training in this technique.
7.1. How to Locate a GBT-Certified Dentist
- Ask Your Current Dentist: Your current dentist may offer GBT or be able to recommend a qualified practitioner in your area.
- Search Online Directories: Several online directories list dentists who offer GBT. You can search these directories by location to find a practitioner near you.
- Check with Dental Associations: Dental associations may have directories of members who offer GBT.
- Contact GBT Training Centers: GBT training centers may be able to provide a list of graduates who offer GBT in your area.
7.2. Questions to Ask Potential Practitioners
When interviewing potential GBT practitioners, ask the following questions:
- What is your experience with GBT?
- What training have you received in GBT?
- What equipment do you use for GBT?
- What are your fees for GBT?
- Do you offer any financing options?
- Can you provide references from other patients who have undergone GBT?
7.3. What to Expect During Your First GBT Appointment
During your first GBT appointment, the practitioner will:
- Review your medical and dental history
- Perform a comprehensive oral examination
- Discuss your oral hygiene goals and concerns
- Explain the GBT procedure in detail
- Answer any questions you may have
- Provide a personalized treatment plan
8. Maintaining Your Oral Health After GBT
After undergoing GBT, it’s important to maintain good oral hygiene practices to prevent biofilm from reaccumulating.
8.1. Essential Oral Hygiene Practices
- Brush your teeth twice a day with fluoride toothpaste: Use a soft-bristled toothbrush and brush for at least two minutes each time.
- Floss daily: Floss between your teeth to remove plaque and debris from areas your toothbrush can’t reach.
- Use an antimicrobial mouthwash: An antimicrobial mouthwash can help kill bacteria and reduce plaque levels.
- Clean your tongue: Use a tongue scraper or toothbrush to clean your tongue and remove bacteria.
- Visit your dentist for regular checkups and cleanings: Regular checkups and cleanings are essential for maintaining good oral health.
8.2. Long-Term Benefits of Consistent Oral Care
- Preventing Tooth Decay: Consistent oral care can prevent tooth decay by removing plaque and bacteria that produce acids that attack tooth enamel.
- Preventing Gum Disease: Consistent oral care can prevent gum disease by removing plaque and bacteria that cause inflammation and infection of the gums.
- Maintaining Fresh Breath: Consistent oral care can help maintain fresh breath by removing bacteria and debris that cause bad odor.
- Protecting Your Overall Health: Good oral health is linked to overall health. Consistent oral care can help protect you from systemic diseases such as diabetes, cardiovascular disease, and respiratory infections.
9. Addressing Common Concerns About GBT
It’s natural to have questions and concerns about a new treatment like GBT. Here, we address some common concerns to help you feel more confident.
9.1. Is GBT Safe for Everyone?
GBT is generally safe for most patients, but there are some exceptions. Patients with certain medical conditions, such as respiratory problems or sensitivity to air polishing powders, may not be good candidates for GBT. It’s important to discuss your medical history with your dentist before undergoing this procedure.
9.2. What is the Long-Term Effectiveness of GBT?
Studies have shown that GBT can be effective in reducing plaque levels, gingival inflammation, and probing depths. However, the long-term effectiveness of GBT depends on the patient’s adherence to good oral hygiene practices and regular maintenance appointments.
9.3. How Does GBT Compare to Other Biofilm Removal Methods?
GBT offers several advantages over traditional methods of biofilm removal, including enhanced patient comfort, improved efficiency, minimized damage to tooth structure, and effective biofilm removal in hard-to-reach areas. However, GBT may not be as effective as SRP in cases with severe calculus accumulation or advanced periodontal disease.
9.4. Potential Side Effects and How to Manage Them
Some patients may experience temporary sensitivity or irritation after GBT. These side effects are usually mild and resolve within a few days. Your dentist may recommend using a desensitizing toothpaste or mouthwash to help manage any discomfort.
10. The Future of Guided Biofilm Therapy
GBT is a rapidly evolving field, and new research and technologies are constantly emerging.
10.1. Emerging Technologies in Biofilm Management
- Laser Therapy: Laser therapy is being investigated as a potential adjunct to GBT for biofilm removal and periodontal treatment.
- Antimicrobial Agents: New antimicrobial agents are being developed to target specific bacteria in the biofilm and prevent its formation.
- Probiotics: Probiotics are being explored as a way to restore a healthy balance of bacteria in the oral cavity and prevent biofilm formation.
- Artificial Intelligence: AI is being used to develop personalized oral hygiene recommendations and improve the efficiency of biofilm removal.
10.2. The Role of GBT in Preventive Dentistry
GBT is playing an increasingly important role in preventive dentistry by helping patients maintain good oral health and prevent tooth decay and gum disease. By targeting biofilm early and effectively, GBT can help reduce the need for more invasive and costly treatments in the future.
10.3. How GBT is Changing Dental Practices
GBT is changing dental practices by shifting the focus from traditional scaling methods to gentle, minimally invasive techniques. This is leading to improved patient comfort, increased efficiency, and better long-term outcomes.
Conclusion: Embracing a Modern Approach to Oral Health
Is guided biofilm therapy worth it? Guided Biofilm Therapy represents a significant advancement in the field of preventive dentistry, offering a gentle, efficient, and effective method for biofilm management. By prioritizing patient comfort, preserving tooth structure, and promoting patient education, GBT can help you achieve and maintain optimal oral health for life.
For more detailed information, personalized guidance, and to explore further resources on maintaining optimal oral health, visit CONDUCT.EDU.VN today. Our platform provides expert advice and practical solutions tailored to your unique needs.
Address: 100 Ethics Plaza, Guideline City, CA 90210, United States
WhatsApp: +1 (707) 555-1234
Website: CONDUCT.EDU.VN
Take the first step towards a healthier smile by visiting conduct.edu.vn and discovering how GBT and our comprehensive resources can transform your oral health routine.
FAQ About Guided Biofilm Therapy
-
What is Guided Biofilm Therapy (GBT)?
GBT is a systematic approach to removing dental biofilm (plaque) using a series of steps, including assessment, disclosing, motivation, air polishing, perio-flow, and scaling (if needed). -
How does GBT differ from traditional scaling and root planing (SRP)?
GBT uses gentle, minimally invasive techniques like air polishing, while SRP involves manual scraping. GBT is often more comfortable and efficient. -
Is GBT safe for everyone?
GBT is generally safe, but individuals with respiratory issues or powder sensitivities should consult their dentist first. -
What are the benefits of GBT?
Benefits include enhanced comfort, efficiency, minimized damage to tooth structure, and effective biofilm removal in hard-to-reach areas. -
How often should I undergo GBT?
The frequency depends on your oral health needs; your dentist will recommend a personalized schedule. -
Does GBT remove stains from teeth?
Yes, air polishing in GBT is effective at removing stains and discoloration from tooth surfaces. -
Can GBT treat periodontal disease?
GBT can be part of the treatment for periodontal disease, particularly in managing biofilm in periodontal pockets. -
Is GBT more expensive than traditional cleaning methods?
GBT may be more expensive initially due to specialized equipment and training, but the long-term benefits can outweigh the costs. -
How do I find a qualified GBT practitioner?
Ask your dentist, search online directories, or check with dental associations for GBT-certified professionals. -
What can I expect during my first GBT appointment?
Expect a comprehensive oral examination, a discussion of your oral hygiene goals, and a detailed explanation of the GBT procedure.
