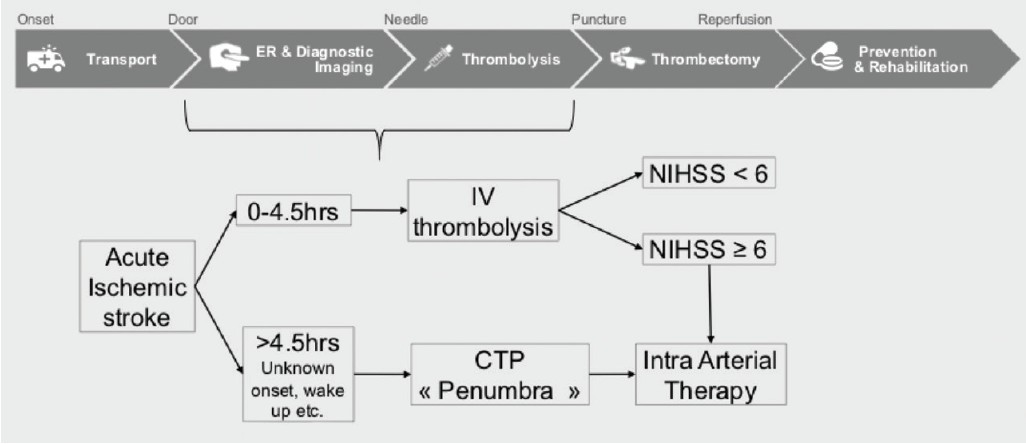
Improving outcomes for stroke patients is critically dependent on the speed of treatment delivery. At Valley Baptist, we implemented the STEPS-T program—Stroke Triage Education, Procedure Standardization, and Technology—to reduce door-to-recanalization times. This initiative begins with stroke triage education, establishing a standardized workflow upon patient arrival. This workflow, guided by the time from symptom onset, directs patients to appropriate imaging and therapies (Figure 1).
Figure 1. Streamlined stroke care pathway for efficient treatment.
Procedure standardization, the second key component, is initiated upon diagnosing a large vessel occlusion requiring intra-arterial therapy (Figure 2). This involves a team-based approach with parallel task execution. Tech 1 prepares the room, devices, and patient, while Tech 2 retrieves data and initiates recording. The nurse manages drug administration and patient monitoring. The neurointerventionalist obtains consent and ensures correct table positioning. The focus during the procedure is safe and efficient thrombectomy.
Figure 2. Standardized procedure workflow for intra-arterial stroke therapy.
Technology optimization is the final critical element. Customized and automated imaging protocols eliminate the need for adjustments during procedures. An advanced monitoring and recording system is in place for data collection. Furthermore, we have adopted a thrombectomy approach utilizing next-generation technology to enhance angiographic and clinical outcomes and improve puncture-to-revascularization times.
For thrombectomy, we employ combination therapy using the ACE™ 68 Reperfusion Catheter and the 3D™ Revascularization Device from Penumbra, Inc. Early research and recent studies support the benefits of combining aspiration and stent retriever techniques. A German study highlighted the advantages of aspiration in combination therapy, demonstrating an 86% reperfusion rate compared to 65% with stent retriever and balloon guide groups. Regression analysis indicated a 3.48 odds ratio favoring combination therapy over stent retriever and balloon guide catheter techniques. The combination approach also showed a trend toward reduced emboli to new territories.
Further evidence supporting aspiration, both as a primary approach and in combination, was presented at the International Stroke Conference 2018. The COMPASS trial compared direct aspiration first-pass technique (ADAPT) as a frontline strategy against a stent retriever frontline (SRFL) approach. Notably, 87% of the SRFL arm used a reperfusion catheter, predominantly the ACE68. Preliminary COMPASS trial results indicated promising revascularization rates (mTICI 2b/3) of 91.7% and 89% for aspiration and stent retriever groups respectively (P = .054). Functional outcomes at 90 days showed 52% for aspiration and 49% for stent retriever groups (P = .0014 for noninferiority).
Aspiration clearly plays a vital role in achieving excellent angiographic and functional outcomes in stroke treatment.
Next-Generation Stroke Technology: The Penumbra 3D Revascularization Device
Penumbra’s 3D Revascularization Device, launched in summer 2017, represents a significant advancement in ischemic stroke treatment. This next-generation retrieval device features a unique architecture with four intraluminal chambers. These chambers are designed to centrally lock the clot within the device, facilitating its withdrawal into the ACE68 catheter. This design offers several key advantages:
- The 3D device can be retracted into and through the ACE68.
- ACE68 access can be maintained at the occlusion site.
- Potential for reduced clot shearing during withdrawal into ACE68.
These benefits enable efficient 3D deployment and retrieval and pave the way for a novel technique called COMPLETE. COMPLETE employs alternating aspiration and 3D mechanisms for efficient clot engagement and removal. If clot persists after 3D withdrawal through ACE68, aspiration can be applied directly at the clot face with ACE68 to finalize the recanalization. COMPLETE offers the advantage of utilizing two proven mechanical thrombectomy techniques based on aspiration.
Case Reports: Clinical Experience with Penumbra 3D and ACE™ 68
Case 1: Internal Carotid Artery (ICA) and M1 Occlusion
By Ameer E. Hassan, DO, FAHA, FSVIN
A patient presented with an ICA occlusion extending past the carotid bulb (Figure 1). Access was achieved using a Neuron™ MAX 088 long sheath (Penumbra, Inc.), and the ACE68 catheter was used to aspirate the ICA clot. Following ICA clearance, an M1 occlusion remained (Figure 2). The 3D device, in conjunction with ACE68, was used to retrieve an organized clot from the M1. The final result was mTICI 3 recanalization (Figure 3), with the clot successfully captured within the 3D intraluminal chamber (Figure 4).
Figure 1. Pre-operative imaging showing Internal Carotid Artery occlusion.
Figure 2. Angiogram showing remaining M1 occlusion post ICA clearance.
Figure 3. Excellent mTICI 3 post-procedure outcome achieved.
Figure 4. Retrieved clot locked within the Penumbra 3D device’s chamber.
Case 2: M1 Occlusion with Tortuous Anatomy
By Ian Kaminsky, MD
At our center, the standard first-line approach is ADAPT, typically using three aspiration-only passes before considering a stent retriever. While aspiration alone is successful in over 85% of cases, stent retrievers are used as adjunctive therapy or to aid ACE68 tracking.
In this case, a patient presented with an M1 origin occlusion and significant ICA tortuosity (Figure 1). Due to proximal vessel tortuosity, the Neuron MAX sheath, hubbed at the femoral sheath, barely reached the carotid bulb, hindering ACE68 advancement beyond the ophthalmic artery. The 3D device was introduced and used as an access tool to “grapple hook” the ACE68 to the clot face. Retraction of 3D through ACE68 partially removed the M1 clot, opening the origin. With ACE68 positioned in the M1, a rapid transition to aspiration alone completed the recanalization, resulting in mTICI 2C (Figure 2 and Figure 3). The COMPLETE technique facilitated a seamless transition between 3D and aspiration.
Figure 2. Proximal M1 occlusion successfully opened using Penumbra 3D.
Figure 3. Final M1 recanalization achieved with aspiration following 3D intervention.
Case 3: ADAPT and 3D for M1 Occlusion – Experience of Zeguang Ren, MD, PhD
By Zeguang Ren, MD, PhD
Since 2012, I have utilized the ADAPT approach, finding it highly effective for most stroke cases. We have recently incorporated the new 3D Revascularization Device for cases where aspiration alone is insufficient to achieve mTICI 2b/3 revascularization. The 3D device’s unique intraluminal chamber architecture represents a significant departure from previous-generation stent retrievers, effectively locking the clot within the device, as demonstrated in this case.
In this instance, we treated an M1 occlusion with ADAPT (Figure 1). After several passes with the ACE™ 64 (Penumbra, Inc.), we introduced 3D through the ACE64 catheter to extract the clot. 3D was delivered via a Velocity® microcatheter (Penumbra, Inc.), which was then removed before initiating aspiration with ACE64 and Pump MAX™ (Penumbra, Inc.). A single pass with 3D resulted in the retrieval of a highly organized clot, cleanly locked within the intraluminal chamber (Figure 2 and Figure 3).
Figure 2. Post-procedure angiographic result after thrombectomy.
Figure 3. Retrieved thrombus cleanly locked inside the Penumbra 3D device.
Case 4: Distal Carotid and Middle Cerebral Artery Occlusion
By H. Robert Hixson, MD
ACE68 is our primary device for stroke thrombectomy, yielding excellent outcomes in most cases. Previously, when stent retrievers were necessary, we typically used traditional stent designs with peripheral metallic tines.
This case involved a distal carotid and middle cerebral artery occlusion (Figure 1). Such cases can be challenging due to substantial clot burden. Initial suction thrombectomy attempts using Neuron MAX, ACE68, and a Velocity microcatheter yielded minimal success despite multiple passes. A traditional stent retriever with concurrent aspiration was also ineffective. Recognizing the unique intraluminal chamber design of the 3D device, we employed it with concurrent aspiration. The 3D device successfully captured a significant thrombus burden, demonstrating impressive performance (Figure 2 and Figure 3).
Figure 2. Post-procedure result after using Penumbra 3D device.
Figure 3. Significant clot burden effectively captured by the 3D Revascularization Device.
Disclaimer: The clinical experiences and opinions presented are for informational purposes only and may not be predictive for all patients. Individual results can vary.