Abstract
Therapeutic approaches using mindfulness meditation are gaining traction, yet the brain mechanisms behind them remain largely unexplored. Mindfulness-Based Stress Reduction (MBSR), a leading program, is known for its positive impact on mental well-being and symptom relief across various conditions. This longitudinal study investigates how MBSR affects brain gray matter concentration. We used anatomical MRI to scan sixteen meditation-naïve individuals before and after an eight-week MBSR course, comparing them to a control group of seventeen. Voxel-based morphometry analysis revealed increased gray matter in the left hippocampus within the MBSR group, confirming our region of interest hypothesis. Whole-brain analysis further identified increases in the posterior cingulate cortex, temporo-parietal junction, and cerebellum. These findings suggest MBSR participation is linked to structural brain changes in areas critical for learning, memory, emotional regulation, self-awareness, and perspective-taking, offering valuable insights into the Structure Of Matter-study Guide 8 of the brain and mind connection.
Keywords: meditation, mindfulness, voxel based morphometry, gray matter, longitudinal, hippocampus, posterior cingulate, structure of matter-study guide 8
1. Introduction
Mindfulness meditation’s benefits extend beyond meditation sessions, positively impacting psychological well-being. Over the past three decades, mindfulness practices have been increasingly integrated into psychotherapy to leverage these advantages (Baer, 2003; Grossman et al., 2004). Research has shown mindfulness-based interventions effectively reduce symptoms of anxiety (Roemer et al., 2008), depression (Teasdale et al., 2000), substance abuse (Bowen et al., 2006), eating disorders (Tapper et al., 2009), and chronic pain (Grossman et al., 2007), while enhancing well-being and life quality (Carmody and Baer, 2008). Mindfulness meditation cultivates present-moment awareness with compassion and non-judgment (Kabat-Zinn, 1990), fostering a perceptual shift (Carmody, 2009) where thoughts and feelings are seen as events within a broader awareness. Understanding this shift is crucial for anyone seeking a structure of matter-study guide 8 for their mental well-being.
Neuroimaging studies are now exploring mindfulness’s neural underpinnings using EEG (Davidson et al., 2003; Slagter et al., 2007) and fMRI (Farb et al., 2007; Lutz et al., 2008; Farb et al., 2010; Goldin and Gross, 2010). Cross-sectional anatomical MRI studies reveal experienced meditators have distinct gray matter morphometry in several brain regions compared to non-meditators (Lazar et al., 2005; Pagnoni and Cekic, 2007; Hölzel et al., 2008; Luders et al., 2009; Vestergaard-Poulsen et al., 2009; Grant et al., 2010). While findings vary across studies due to participant diversity, meditation types, and analysis methods (see Table 1), the hippocampus and right anterior insula show consistent differences, with activation in both regions during meditation (hippocampus (Lazar et al., 2000; Hölzel et al., 2007); insula (Farb et al., 2007; Lutz et al., 2008)). The hippocampus is vital for learning and memory (Squire, 1992) and emotional control modulation (Corcoran et al., 2005; Milad et al., 2007), while the insula is thought to be key in awareness (Craig, 2009), functions central to mindfulness training (Bishop et al., 2004; Shapiro et al., 2006; Ortner et al., 2007).
Table 1.
Overview of morphometric studies on meditation
| Study | Meditation tradition | N Meditators/Controls | Morphological measures | Regions identified greater in meditators than controls |
|---|---|---|---|---|
| Lazar et al. (2005) | Insight | 20 / 15 | Cortical thickness | Right anterior insula and right middle and superior frontal sulci |
| Pagnoni & Cekic (2007) | Zen | 13 / 13 | Gray matter volume (VBM in SPM5) | Meditators showed no age-related decline in the left putamen as compared to controls |
| Hölzel et al. (2008) | Insight | 20 / 20 | Gray matter density (VBM in SPM2) | Left inferior temporal lobe, right insula, and right hippocampus |
| Vestergaard-Poulsen et al., (2009) | Tibetan Buddhist | 10 / 10 | Gray matter density & volume (VBM in SPM5) | Medulla oblongata, left superior and inferior frontal gyri, anterior lobe of the cerebellum and left fusiform gyrus |
| Luders et al. (2009) | Zazen, Vipassana, Samatha & others | 22 / 22 | Gray matter volume (VBM in SPM5) | Right orbito-frontal cortex, right thalamus, left inferior temporal lobe, right hippocampus |
| Grant et al. (2010) | Zen | 19/20 | Cortical thickness | Right dorsal anterior cingulate cortex, secondary somatosensory cortex |
VBM: voxel-based morphometry (Gaser), SPM: Statistical Parametric Mapping, (Wellcome Department of Cognitive Neurology, London)
Neural systems are known to be adaptable, with adult brain structure changing through training. Longitudinal studies show task-specific gray matter increases from learning abstract information (Draganski et al., 2006), motor skills (Draganski et al., 2004), aerobic training (Colcombe et al., 2006), and cognitive skills (Ilg et al., 2008). Cross-sectional studies link regional gray matter differences to performance abilities (Mechelli et al., 2004; Milad et al., 2005), suggesting increased gray matter improves function in relevant areas. Studies on experienced meditators hint at structural plasticity, but cross-sectional designs can’t confirm causality due to potential pre-existing differences. Our longitudinal study examines gray matter changes from mindfulness intervention, focusing on an eight-week Mindfulness-Based Stress Reduction course (MBSR; Kabat-Zinn, 1990). This program aims to enhance mindfulness, well-being, and reduce perceived stress. We sought objective neurological changes underlying mindfulness practice’s trait changes, using voxel-based morphometry to investigate gray matter concentration changes, with a focus on the hippocampus and insula as predefined regions of interest, and exploratory whole-brain analyses compared to a control group.
2. Methods
2.1 Participants
MBSR participants were recruited from MBSR courses at the Center for Mindfulness at the University of Massachusetts Medical School, including physician and self-referred individuals seeking stress reduction from across New England. Inclusion criteria were: physical and psychological health, no medications, limited prior meditation experience (no classes in past six months, ≤ four classes in past five years, or ≤ ten lifetime classes), age 25-55, MRI compatibility, and commitment to full course attendance and homework. Eighteen healthy, right-handed individuals (8 male, 10 female, mean age 37.89 years, SD 4.04 years) were enrolled. Two dropped out after the first MRI due to discomfort, leaving a final sample of 16 (6 male, 10 female, mean age 38.0 years, SD 4.1 years). Ethnicities included 13 Caucasians, one Asian, one African American, and one multi-ethnic, with an average education of 17.7 years (SD 1.9 years). Participants received a discounted MBSR course fee as reimbursement.
The control group consisted of 17 participants (11 male, 6 female, mean age 39.0 years, SD 9.2 years, average education 17.3 years, SD 1.8 years). Ethnicities were 13 Caucasians, two Asians, two African Americans, and one Hispanic. No significant differences in age (t(22.3) = .56; p = .58) or education (t(30) = −.56, p = .58) were found between groups. The study protocol was approved by the IRBs of Massachusetts General Hospital and the University of Massachusetts Medical School, and all participants provided written informed consent. Data from this sample was previously used in a publication on neural correlates of perceived stress changes (Hölzel et al., 2009).
2.2 Intervention
The MBSR program, detailed elsewhere (Kabat-Zinn, 1990), involves eight weekly 2.5-hour group sessions, plus a 6.5-hour day in week six. It aims to develop mindfulness – present-moment awareness with compassion and non-judgment – through formal exercises like body scan, mindful yoga, and sitting meditation. The body scan guides attention through the body, observing sensations non-judgmentally, culminating in whole-body awareness. Mindful yoga includes gentle stretches and slow, breath-coordinated movements, emphasizing moment-to-moment awareness and body respect. Sitting meditation starts with breath awareness, expanding to sounds, sights, tastes, body sensations, thoughts, and emotions, progressing to open awareness meditation or simple present-moment awareness.
Participants received 45-minute guided audio recordings (body scan, yoga, sitting meditation) for daily home practice. Informal mindfulness in daily activities (eating, walking, washing dishes, showering, etc.) was also taught. Classes included formal practice, discussions on applying mindfulness to daily life, and didactic instruction on stress coping using mindfulness. MBSR participants historically show varied home practice compliance, so participants recorded daily mindfulness exercise time.
2.3 Five Facet Mindfulness Questionnaire
The Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006), a 39-item scale, measures five mindfulness facets: Observing (noticing internal/external stimuli), Describing (labeling stimuli with words), Acting with Awareness (attending to current actions vs. automatic behavior), Non-judging of Inner Experience (refraining from evaluating sensations, cognitions, emotions), and Non-reactivity to Inner Experience (allowing thoughts/feelings to pass without engagement). Items are rated on a 5-point Likert scale (1=never/rarely true, 5=very often/always true). Subscales show adequate to good internal consistency (Baer et al., 2006). Usable data from both time points were collected from 14 MBSR and 14 control participants.
2.4 MRI data collection and analysis
All participants were scanned at the Martinos Center for Biomedical Imaging in Charlestown, MA, using a Siemens Magnetom Avanto 1.5 T scanner with a standard head coil. MBSR participants were scanned within two weeks before (Pre) and after (Post) the program. Control scans were about two months apart (average 56.25 days, SD 4.5 days for MBSR; 65.67 days, SD 11.22 days for controls). High-resolution MRI data were acquired using a T1-weighted MPRAGE sequence (128 sagittal slices, 1.0 × 1.0 × 1.3 mm, TI = 1000 ms; TE = 3.39 ms; TR = 2730 ms). Image analysis was performed with voxel-based morphometry (VBM) tools in SPM5 (www.fil.ion.ucl.ac.uk/spm/software/spm5/), based in MATLAB 7.1, using default settings unless specified. VBM allows automated voxel-wise whole-brain statistical MRI scan comparisons (Ashburner and Friston, 2000). Images were manually aligned to the anterior commissure, then segmented into gray and white matter in native space using SPM5’s ‘Native Space’ segmentation. For each participant, Pre and Post gray matter segmentations were spatially co-registered. Normalization parameters were calculated for the Pre scan and applied to both time points (trilinear interpolation, 2 × 2 × 2 mm) to avoid removing regional differences through scan-specific spatial normalization (Driemeyer et al., 2008; Ilg et al., 2008). Images were smoothed with an 8 mm full width at half maximum Isotropic Gaussian Kernel.
Exploratory whole-brain and region of interest (ROI) analyses were conducted. ROI (bilateral hippocampi and insulae) was created using WFU Pickatlas software (Maldjian et al., 2003) based on Tzourio-Mazoyer et al. parcellation (Tzourio-Mazoyer et al., 2002). A paired t-test within the MBSR group in SPM5 identified brain regions with significantly increased gray matter concentration post-MBSR. ROI analysis used voxel-wise correction for multiple comparisons within the ROI. Whole-brain analysis used a cluster-wise method, corrected for multiple comparisons across the brain using SPM5 (Friston et al., 1994), with a cluster size threshold of 250 voxels and initial voxel-level threshold of p < .01, uncorrected. Significance was set at p < .05, corrected for multiple comparisons for both analyses.
Values from identified clusters were extracted for each participant and time point using Marsbar toolbox (Brett et al., 2002). Repeated measures ANOVA was performed for each cluster in SPSS, with group (MBSR/control) as between-subjects and time-point (Pre/Post) as within-subjects factor, controlling for age and gender as nuisance variables.
3. Results
3.1 Amount of mindfulness practice
MBSR participants reported an average of 22.6 hours (SD: 6.3 hours) of formal homework exercises over eight weeks (average 27 minutes/day). Body scan practice ranged from 335 to 1002 minutes (mean: 699 min, SD: 217 min), yoga from 103 to 775 minutes (mean: 327 min, SD: 194 min), and sitting meditation from 0 to 755 minutes (mean: 332 min, SD: 211 min). No significant correlations were found between practice types: body scan and yoga (r = −0.042, P = 0.87), body scan and sitting (r = −0.26, P = 0.33), yoga and sitting (r = 0.49, P = 0.06, N = 16).
3.2 Improvements in mindfulness
Repeated measures ANOVAs showed significant group-by-time interactions for three mindfulness subscales: acting with awareness (F(1,26) = 16.87, P < 0.001), observing (F(1,26) = 7.09, P = 0.013), and non-judging (F(1,26) = 4.61, P = 0.041). Describing (F(1,26) = 1.95, P = 0.175) and non-reactivity (F(1,26) = 2.79, P = 0.107) showed no significant interactions. Paired t-tests confirmed significant increases in the MBSR group for acting with awareness (t(13) = 3.665, P = 0.003), observing (t(13) = 4.218, P = 0.001), and non-judging (t(13) = 3.580, P = 0.003), but not in the control group (observing: t(13) = −0.698, P = 0.498; acting with awareness: t(13) = −1.991, P = 0.068; non-judging: t(13) = 0.657, P = 0.523; two-tailed). MBSR participants significantly improved mindfulness scores on these three scales.
3.3 Gray matter changes in a priori regions of interest
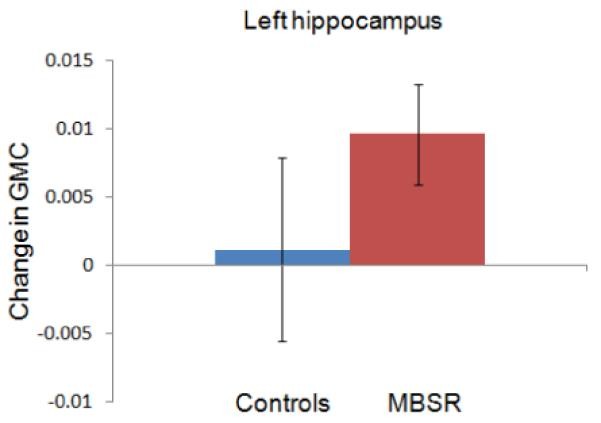
The paired t-test in the MBSR group identified a small left hippocampus cluster with increased gray matter concentration (peak MNI coordinates x, y, z: −36, −34, −8; t(15) = 6.89; voxel level P = 0.014, FWE corrected; cluster size k = 30; Figure 1).
Figure 1.
Alt Text: Figure 1: Region of interest analysis showing increased gray matter concentration in the left hippocampus of the MBSR group. MNI coordinates are displayed for axial (1A), sagittal (1B), and coronal (1C) views. Graph 1D shows the change in gray matter concentration (GMC) within the left hippocampus cluster from pre to post-MBSR intervention for both MBSR and control groups, with 95% confidence intervals. This visual guide enhances the structure of matter-study guide 8 concept by showing tangible brain changes.
Average gray matter concentration in this cluster was extracted for each individual at each time point and analyzed in SPSS. Repeated measures ANOVA (2 groups × 2 time-points, controlling for age and gender) showed a significant group x time interaction (F(1,29) = 4.92; P = .035). No baseline difference in gray matter concentration was found between groups at the Pre time point (t(31) = .06; P = .956), and the control group showed no change from Pre to Post (t(16) = .343; P = .736). Pre-Post changes in other ROIs were not significant, nor were changes in a priori regions correlated with homework practice or FFMQ changes. Paired t-test within the control group showed no significant gray matter changes. ROI analysis confirmed significant left hippocampus increases in the MBSR group, indicating structural changes in this region within eight weeks of mindfulness training.
3.4 Whole brain analysis
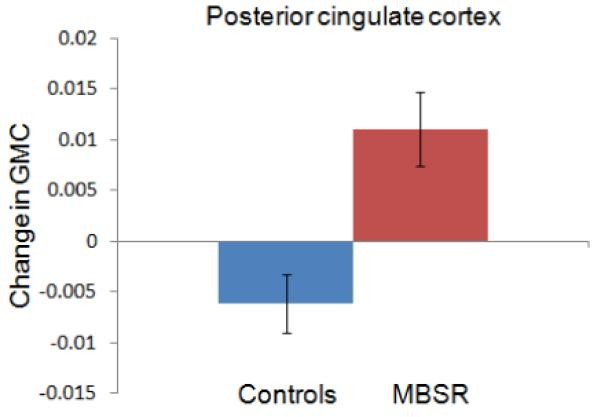
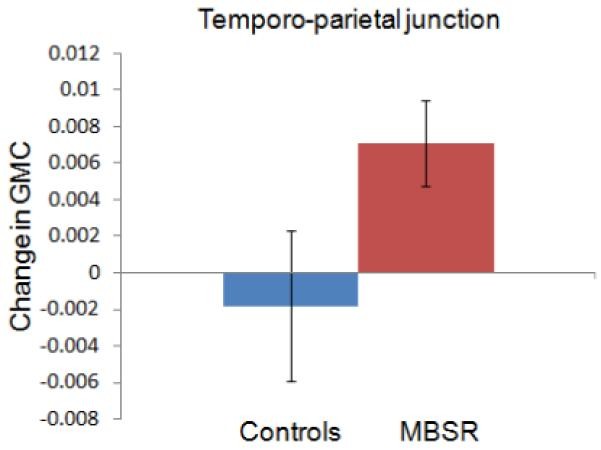
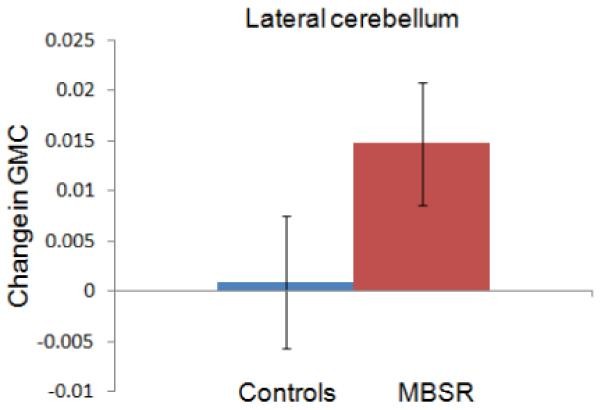
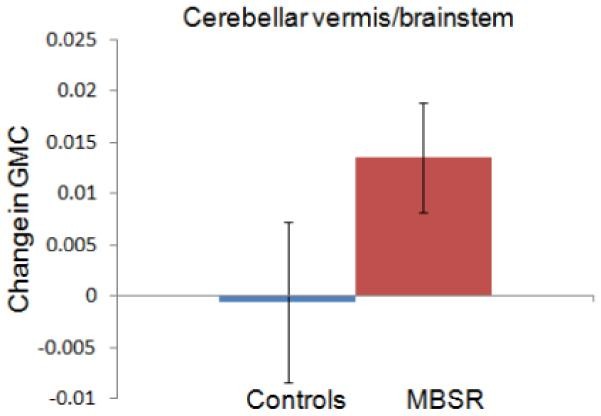
Exploratory whole-brain analysis (paired t-test in SPM5) revealed four clusters with significantly greater gray matter concentration post-MBSR (Table 2). One cluster was in the posterior cingulate cortex (PCC; Figure 2A, 3A), one in the left temporo-parietal junction (TPJ; Figure 2B, 3B), and two in the cerebellum (Figures 2A and C, 3 C and D). One cerebellar cluster was centered in the vermis, extending into the brainstem, encompassing pontine nuclei. The other was lateral, including parts of the left lobule X and VIII (lateral posterior and flocculonodular lobe). No regions showed decreased gray matter concentration after MBSR.
Table 2.
Increase in gray matter concentration from Pre- to Post-MBSR training in the exploratory whole brain analysis within the MBSR group
| Region (peak of cluster) | Cluster size k | Cluster-level P-value | MNI coordinates of the peak voxel (x, y, z) | T of peak voxel |
|---|---|---|---|---|
| Posterior cingulate gyrus | 418 | 0.004 | −4, −34, 32 | 5.07 |
| Cerebellum Lobule 8 – L | 329 | 0.018 | −28, −38, −48 | 5.31 |
| Cerebellum, Vermis, Lobule 1-2 | 499 | 0.001 | 4, −40, −24 | 5.03 |
| Temporo-parietal junction (peak in middle temporal gyrus) | 291 | 0.036 | −50, −48, 20 | 5.08 |
P-values are corrected for multiple comparisons for the whole brain.
Figure 2.
Alt Text: Figure 2: Whole brain analysis showing increased gray matter concentration in the MBSR group from pre to post-intervention. Image A displays clusters in the posterior cingulate cortex and cerebellum (sagittal view). Image B shows the cluster in the left temporo-parietal junction (sagittal view). Image C highlights clusters in the cerebellum and brainstem (axial view). Significant clusters are overlaid on a group-averaged structural MPRAGE image, illustrating the structure of matter-study guide 8 in brain changes.
Figure 3.
Alt Text: Figure 3: Graphs depicting the change in gray matter concentration (GMC) for MBSR and control groups in four key brain regions. 3A: Posterior cingulate cortex. 3B: Temporo-parietal junction. 3C: Lateral cerebellum. 3D: Cerebellar vermis/brainstem. Error bars represent 95% confidence intervals, visually representing the structure of matter-study guide 8 data on brain plasticity.
Averaged values for each cluster were extracted and analyzed using repeated measures ANOVAs (2 groups × 2 time-points) with age and gender as covariates. Significant group x time interactions were found for all four regions, indicating greater gray matter concentration increases in the MBSR group: PCC (F(1,29) = 50.124; P < .001), TPJ (F(1,29) = 11.456; P = .002), cerebellar vermis/brainstem (F(1,29) = 11.292; P = .002), and lateral cerebellum (F(1,29) = 9.806; P = .004).
Gray matter concentration changes in the control group were not significant for TPJ (t(16) = −.87; P = .40), cerebellar vermis (t(16) = −.15; P = .88), or lateral cerebellum (t(16) = .273; P = .79). However, a decrease was observed in the PCC cluster (t(16) = −4.121; P = .001). Baseline group comparisons at the Pre time point showed no significant differences in PCC (t(31) = .24; P = .81), TPJ (t(31) = .85; P = .40), and lateral cerebellum (t(31) = .−1.41; P = .17), but the control group had greater gray matter concentration in the cerebellar vermis cluster (t(31) = 2.84; P = .008). Homework practice and FFMQ changes were not correlated with cluster changes. Control group paired t-test showed no significant gray matter changes. Exploratory analyses indicate MBSR-related gray matter increases in the PCC, TPJ, and cerebellum, suggesting MBSR course participation causes structural changes in these brain regions, further illuminating the structure of matter-study guide 8 of the brain.
4. Discussion
This study demonstrates longitudinal increases in brain gray matter concentration following an eight-week MBSR course compared to a control group. Our hypothesis of left hippocampus gray matter concentration increase was confirmed. Exploratory whole-brain analysis revealed significant increases in the PCC, TPJ, and cerebellum.
The hippocampus is thought to mediate meditation benefits due to its role in cortical arousal and responsiveness (Newberg and Iversen, 2003), with previous studies showing morphological hippocampus differences between meditators and non-meditators (Hölzel et al., 2008; Luders et al., 2009). The hippocampus also regulates emotion (Corcoran and Maren, 2001; Corcoran et al., 2005; Milad et al., 2007, and structural changes may reflect improved emotional regulation. Conversely, conditions like major depression (Sheline, 2000) and PTSD (Kasai et al., 2008) are linked to decreased hippocampal density/volume, potentially due to neuronal loss, glial cell loss, reduced neurotrophic factors, or neurogenesis reduction (Sheline, 2000). Smaller hippocampi are also a risk factor for stress-related psychopathology (Gilbertson et al., 2002). However, the hippocampus can remodel synapses and generate new neurons (Gage, 2002), and volume loss may be reversible (Gould et al., 2000; Jacobs et al., 2000). Antidepressants, like SSRIs, can increase hippocampal volume (Vermetten et al., 2003), with some behavioral effects potentially linked to hippocampal neurogenesis (Santarelli et al., 2003). Future research should explore if similar neural mechanisms underlie mental health improvements from medication-free interventions like MBSR. While previous work with this sample linked perceived stress changes to amygdala structural changes, not hippocampus (Hölzel et al., 2009), hippocampus changes here may relate to other well-being improvements reported after MBSR. This deeper understanding contributes to our structure of matter-study guide 8 of brain health.
The insula is involved in interoceptive awareness (Critchley et al., 2004) and empathy (Singer et al., 2004), with a central role in human awareness or consciousness (Craig, 2009). Given mindfulness training’s focus on interoception and conscious awareness, and previous findings of insula differences in meditators (Hölzel et al., 2008; Lazar et al., 2005; Lutz et al., 2008), we hypothesized structural increases, but Pre-Post MBSR comparison was not significant. More practice might be needed for insula structural changes. Pre-existing differences, not training, might explain prior meditator-non-meditator differences. A recent study also challenged the link between meditator insula changes and interoceptive ability (Khalsa et al., 2008). Future studies with longer training and interoceptive awareness assessments are needed to resolve these contradictions and refine our structure of matter-study guide 8 understanding.
The TPJ is crucial for self-consciousness, mediating spatial self-body unity (Blanke et al., 2005) or embodiment (Arzy et al., 2006, with TPJ impairment potentially leading to disembodiment (Blanke et al., 2005). It’s also involved in social cognition, inferring others’ mental states (Van Overwalle, 2009), and shows greater activation during compassion in meditators (Lutz et al., 2008). Mindfulness training cultivates self-awareness as a ‘complete whole’ (Kabat-Zinn, 1990) and compassion. TPJ morphological changes might relate to increased compassion from meditation (Shapiro et al., 2005) and embodied self-cultivation, enhancing our grasp on the structure of matter-study guide 8 of self-perception.
The PCC is engaged when assessing stimulus relevance to oneself (Schmitz and Johnson, 2007), integrating self-referential stimuli into emotional and autobiographical context (Northoff and Bermpohl, 2004). These functions align with mindfulness practice’s introspective observation of experiences (Kabat-Zinn, 1990). Structural increases may relate to repeated PCC activation during this process. Interestingly, the hippocampus, TPJ, and PCC (plus medial prefrontal cortex parts not found here) form a network (Vincent et al., 2006) supporting self-projection (Buckner and Carroll, 2007), including remembering the past, future thinking (Schacter et al., 2007), and perspective-taking (Saxe and Kanwisher, 2003). These abilities may share processes using autobiographical information to perceive alternative perspectives (Buckner and Carroll, 2007). Mindfulness mechanisms literature suggests benefits arise from a perceptual shift modulating self-representation (Shapiro et al., 2006; Carmody, 2009, and structural changes in this self-projection network might underlie this shift, providing a deeper structure of matter-study guide 8 of cognitive flexibility.
Cerebellar clusters were found in lateral posterior/flocculonodular lobe and vermis/brainstem. Beyond sensory integration, coordination, and motor control (Marr, 1969), the cerebellum is crucial for emotion and cognition regulation. Cerebellar lesions can cause the “cerebellar cognitive affective syndrome” (Schmahmann et al., 2007). The cerebellum may regulate cognitive and emotional process speed, capacity, consistency, and appropriateness (Schmahmann, 2004, modulating behavior around a homeostatic baseline. Given emotion and cognition regulation’s importance in psychological health, cerebellar morphological changes may contribute to mindfulness’s well-being benefits, enriching our structure of matter-study guide 8 of emotional balance.
Brainstem regions, possibly including locus coeruleus, nucleus raphe pontis, pontine tegmentum, and trigeminal nucleus (Naidlich et al., 2009), also showed gray matter increases. These differ from cerebellum/brainstem regions found by Vestergaard-Poulsen et al. (Vestergaard-Poulsen et al., 2009). The locus coeruleus synthesizes norepinephrine, and raphe nuclei release serotonin. Serotonin system modulation is effective for mood and anxiety disorders (e.g., SSRIs; Masand and Gupta, 1999). The locus coeruleus-norepinephrine system optimizes performance by modulating arousal, balancing focused/flexible responses, and selective/scanning attention (Aston-Jones et al., 2000; Aston-Jones and Cohen, 2005. This system is vital in cognitive, affective, and behavioral functions, and clinical dysfunctions (e.g., depression, anxiety, sleep disorders; Aston-Jones, 2002), as well as stress response mediation and antidepressant action (Brady, 1994). MBSR programs improve anxiety and depression (Baer, 2003; Kuyken et al., 2008; Roemer et al., 2008), sleep (Carlson and Garland, 2005; Ong et al., 2009), and attention (Jha et al., 2007. Morphological changes here may contribute to these enhancements, further informing our structure of matter-study guide 8 of neurochemical balance.
While TPJ, PCC, and cerebellum Pre-Post changes were found, previous cross-sectional meditator studies didn’t find group differences in these regions. Small differences undetected in prior studies or transient structural changes maximal during new skill acquisition (Driemeyer et al., 2008) may explain this.
MBSR is multifaceted, and benefits may arise from non-meditation components like social interaction, stress education, or stretching. Exercise increases hippocampal neurogenesis (van Praag et al., 1999. Learning-related structural changes, similar to medical students learning new information (Draganski et al., 2006), are possible. Our study, comparing MBSR to a waitlist control, cannot isolate these component effects. The lack of correlation between gray matter change and homework suggests formal practice minutes aren’t the primary driver, but the MBSR program holistically influences morphology. Active control conditions including mindfulness-unspecific program components (MacCoon et al., 2008) are needed to isolate meditation’s specific effects. Our study focused on stress-seeking individuals, limiting generalization to non-stressed individuals or those with mental disorders. Future studies should test broader populations. Finally, our sample size is small, and replication is needed to solidify our structure of matter-study guide 8 findings.
The adult nervous system is plastic, and brain structure changes with training (Gage, 2002; Draganski et al., 2004; Colcombe et al., 2006; Driemeyer et al., 2008). Increased gray matter is generally linked to repeated region activation (May et al., 2007; Ilg et al., 2008), consistent with meditation-related activation in identified regions (Lou et al., 1999; Lazar et al., 2000; Newberg et al., 2001; Hölzel et al., 2007; Lutz et al., 2008). Cellular mechanisms of training-induced neuroanatomical plasticity are still unclear. MBSR improves psychological health and well-being (Grossman et al., 2004; Carmody et al., 2009). Our data showing morphological increases in mental health-related regions suggests a plausible neural mechanism: enduring brain structure changes supporting improved mental function. Understanding neurobiological mechanisms of behavioral interventions is crucial for their effective and targeted use, and for a comprehensive structure of matter-study guide 8 approach to mental wellness.
Acknowledgement
We thank our participants and the Center for Mindfulness. We thank Daniel McCaffrey and Nik Olendzki for data collection support, and Douglas Greve, Ulrich Ott, and Julie Bates for discussions. Funding was provided by the National Institutes of Health-NCCAM (R21-AT003425-01A2), the British Broadcasting Company, and the Mind and Life Institute (Varela research grant). B.K.H. was supported by a Marie Curie Fellowship, and S.W.L. by NIH funding K01AT00694. Funders had no role in study design, data collection, analysis, publication decisions, or manuscript preparation. The authors declare no conflicts of interest.
Footnotes
Publisher’s Disclaimer: This is an unedited manuscript accepted for publication. It will undergo copyediting, typesetting, and proof review before final publication. Errors may occur during production. All legal disclaimers apply to the journal.