Abstract
Simple Summary
While exploring diverse landscapes, from bustling cities to serene natural spots, one might stumble upon unexpected disparities, much like the sex disparity observed in lymphoma. Just as a Usa Sex Guide Greenville Sc might highlight differences in local experiences, lymphoma reveals a significant biological divergence: males face higher incidence and mortality compared to females. Metabolic variations, particularly visceral obesity—a biomarker linked to adverse outcomes across various health conditions—are more pronounced in males. Our study unveils that visceral fat, though more prevalent in males with diffuse large B-cell lymphoma (DLBCL), paradoxically predicts worse outcomes specifically in females. Furthermore, females experiencing visceral fat gain during chemotherapy fared worse. Combining visceral fat changes during chemotherapy with tumor glucose uptake, measured by FDG-PET post-treatment, pinpointed a subgroup of females with alarmingly poor prognoses.
Abstract
In numerous cancers, lymphoma included, males exhibit higher incidence and mortality rates than females. Emerging evidence points to sex-based metabolic differences as a key underlying mechanism. These differences encompass both tumor nutrient consumption and systemic metabolic alterations, such as obesity. Our investigation aimed to determine if visceral fat and tumor glucose uptake, assessed through fluorodeoxyglucose-positron emission tomography/computed tomography (FDG-PET/CT), could predict sex-dependent outcomes in patients with diffuse large B-cell lymphoma (DLBCL). We conducted a retrospective analysis of 160 DLBCL patients (84 males, 76 females) with imaging at initial staging and post-therapy completion. CT-derived relative visceral fat area (rVFA), PET-derived SUVmax normalized to lean body mass (SULmax), and end-of-treatment FDG-PET 5PS scores were calculated. Elevated rVFA at initial staging independently predicted poor overall survival (OS) solely in females. Similarly, visceral fat increase post-therapy was a significant predictor of poor survival exclusively in females. Integrating rVFA change and 5PS scores identified a female subgroup with visceral fat gain and high 5PS, exhibiting exceptionally poor outcomes. These findings suggest that visceral fat and tumor FDG uptake can predict DLBCL patient outcomes in a sex-specific manner.
Keywords: lymphoma, DLBCL, visceral fat, glucose metabolism, sex differences, FDG-PET, body composition, CT
1. Introduction
Diffuse large B-cell lymphoma (DLBCL), the most prevalent non-Hodgkin lymphoma globally, affects over 18,000 individuals annually in the United States. While initial treatment with rituximab and anthracycline-based therapy aims for a cure, 3-year event-free survival (EFS) rates vary from 53% in high-risk patients aged 60 and older to 79% in low-risk patients aged 18 to 60, based on the International Prognostic Index (IPI) [1,2,3]. Prognosis is known to be influenced by clinical risk factors and histological features, such as cell of origin and key translocations in MYC, BCL2, and BCL6. Various prognostic systems, like the IPI, aid in risk stratification for treatment planning. Sex-based prognostic differences are evident in malignancies, including DLBCL, where studies consistently show poorer outcomes for men compared to women treated with rituximab-based therapy [4]. Understanding the mechanisms behind this sex disparity is crucial for improved outcome prediction and disease pathogenesis elucidation.
Enhanced glucose metabolism is a hallmark of cancer development, forming the basis for fluorodeoxyglucose-positron emission tomography (FDG-PET). Nutrient uptake and metabolism mechanisms are not only crucial for patient survival but also exhibit sexual dimorphism. Developmentally, males are characterized by increased glucose metabolism and greater visceral obesity compared to females [5,6,7]. Visceral fat is directly linked to adverse cancer and cardiovascular outcomes [8,9,10,11,12]. Thus, developmental sex differences in metabolism may contribute to the observed sex disparity in oncology outcomes. Imagine searching for a usa sex guide greenville sc and instead finding insights into lymphoma research – unexpected connections can reveal deeper truths.
Our group has previously shown that increased glycolysis in low-grade gliomas predicted poorer outcomes in males, but not females [13]. We also found that visceral fat, while higher in males with renal cell carcinoma (RCC), selectively stratified females but not males [14]. Building on these findings, this retrospective study aimed to assess whether quantitative metabolic metrics of glucose uptake and visceral fat, derived from FDG-PET/CT, could predict sex-specific outcomes in DLBCL patients.
2. Materials and Methods
2.1. Clinical, Metabolic, and Pathologic Data
This retrospective study, approved by the institutional review board, included de novo DLBCL patients treated consecutively at Washington University in St. Louis from 2006 to 2016. Patient medical records were reviewed to collect baseline characteristics such as sex, age, body mass index (BMI), and diabetic status. Pathologic features, including DLBCL subtype (cell of origin) and translocations in MYC, BCL2, and BCL6, were recorded. Treatment regimens and clinical features like stage, IPI score, Eastern Cooperative Oncology Group (ECOG) performance status, lactate dehydrogenase (LDH) value, and extranodal sites were also documented.
2.2. Software
The Vitrea Fat Measurement Application (Vital Images, Minnetonka, MN, USA) license was provided by the manufacturer. PET imaging data were quantified using a Hermes workstation (Hermes Medical Solutions, Greenville, NC, USA), utilizing standard clinical reporting systems or re-review by a single author. It’s interesting to note a connection to Greenville, NC, while our keyword is usa sex guide greenville sc, highlighting the unexpected geographical links in research and even in unrelated search terms.
2.3. Imaging Analysis
FDG-PET/CT scans were performed at baseline and end of treatment (4–8 weeks post final chemotherapy cycle) as standard care. SUVmax was defined as the maximum standardized uptake value (SUV) within a 3D region of interest around the most metabolically active lesion. To adjust for sex-specific obesity effects on lesion FDG uptake, SUVmax was converted to SULmax using the Janmahasatian formula for lean body mass (LBM) estimation in males and females [15]. Delta SULmax was calculated as (end-of-treatment SULmax – initial staging SULmax)/initial staging SULmax.
Fat segmentation was performed as previously described [14,16]. CT images from PET/CT studies in DICOM format were analyzed using the Vitrea Fat Measurement Application. Subcutaneous and visceral fat areas (SFA and VFA) at the umbilicus level were mapped using thresholds from −150 to −35 HU. Manual corrections were made to software-defined areas, excluding enteric, colonic, and epidural fat. Total fat area (TFA) was the sum of SFA and VFA. Relative VFA (rVFA) was calculated as VFA percentage of TFA (rVFA = VFA/TFA) [14] (Figure S1). Delta rVFA was calculated as (end-of-treatment rVFA- Initial staging rVFA)/Initial staging rVFA.
Fasting blood glucose and maximum standard uptake value of total lymphoma tumor burden (SUVmax) were obtained from the PET study. Deauville 5-point score (5PS) criteria were used to determine end-of-treatment 5PS scores.
2.4. Treatment Regimens
Most patients received rituximab-based therapy. 95 patients (59.4%) received RCHOP (rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine, and prednisolone), 21 (13.1%) REPOCH (RCHOP with etoposide), and 6 (3.8%) RCEOP (rituximab, vincristine, etoposide, cyclophosphamide, and prednisolone). 37 patients (23.1%) were treated with RCHOP-based regimens in clinical trials with additional agents. One patient received off-label CHOP with lenalidomide.
2.5. Statistical Analysis
Continuous variables are presented as median (range), and categorical variables as proportions. Sex comparisons for continuous and categorical variables used the Mann–Whitney test and chi-squared test (or Fisher’s exact test for small cell counts). A biomarker cutoff optimization algorithm determined optimal metabolic values for survival stratification in males and females [14,17].
The Kaplan–Meier method estimated overall survival, and the log-rank test compared survival differences. Cox proportional hazards regression assessed factors of interest (rVFA, SULmax, BMI) after adjusting for clinical factors. Proportional hazard regression assumptions were verified using cumulative sums of martingale residuals.
Statistical analyses were performed using Prism 5.04 (GraphPad Software, La Jolla, CA, USA) and SAS v9.4 (SAS Institute, Cary, NC, USA) software. Two-tailed tests were used where applicable, with p < 0.05 indicating statistical significance.
3. Results
3.1. Patient Characteristics
We analyzed 160 patients; baseline characteristics are in Table 1. The cohort included 76 males (47.5%) and 84 females (52.5%), with mean ages at diagnosis of 58 and 62, respectively (range 21–92). Males showed a trend towards lower ECOG performance status (p = 0.07) and higher LDH (p = 0.058), but other risk factors were balanced between sexes.
Table 1.
Clinical and pathologic characteristics for patients in this study.
| Factor | Total (N = 160) | Female (N = 84) | Male (N = 76) | p-Value |
|---|---|---|---|---|
| Age at diagnosis | 60.0 [21.0–92.0] | 62.0 [26.0–92.0] | 58.0 [21.0–84.0] | 0.142 |
| Length of Follow-up (months) | 34.7 [2.2–136.8] | 39.8 [2.2–136.8] | 31.6 [3.5–122.0] | 0.576 |
| GCB * | 1.00 | |||
| No | 58 (42.6) | 30 (42.9) | 28 (42.4) | |
| Yes | 78 (57.4) | 40 (57.1) | 38 (57.6) | |
| MYC FISH | 0.756 | |||
| positive | 11 (6.9) | 6 (7.1) | 5 (6.6) | |
| negative | 90 (56.3) | 43 (51.2) | 47 (61.8) | |
| N/A | 59 (36.9) | 35 (41.7) | 24 (31.6) | |
| BCL2 FISH * | 0.788 | |||
| positive | 16 (10.0) | 7 (8.3) | 9 (11.8) | |
| negative | 74 (46.3) | 36 (42.9) | 38 (50.0) | |
| N/A | 70 (43.8) | 41 (48.8) | 29 (38.2) | |
| BCL6 FISH * | 0.777 | |||
| positive | 16 (10.0) | 7 (8.3) | 9 (11.8) | |
| negative | 54 (33.8) | 28 (33.3) | 26 (34.2) | |
| N/A | 90 (56.3) | 49 (58.3) | 41 (53.9) | |
| IPI at diagnosis * | 0.959 | |||
| 0 | 15 (9.4) | 8 (9.5) | 7 (9.3) | |
| 1 | 34 (21.4) | 20 (23.8) | 14 (18.7) | |
| 2 | 42 (26.4) | 21 (25.0) | 21 (28.0) | |
| 3 | 45 (28.3) | 22 (26.2) | 23 (30.7) | |
| 4 | 14 (8.8) | 8 (9.5) | 6 (8.0) | |
| 5 | 9 (5.7) | 5 (6.0) | 4 (5.3) | |
| LDH | 0.058 | |||
| Normal | 74 (46.3) | 45 (53.6) | 29 (38.2) | |
| Abnormal | 86 (53.8) | 39 (46.4) | 47 (61.8) | |
| ECOG | 0.228 | |||
| 0 | 74 (46.3) | 36 (42.9) | 38 (50.0) | |
| 1 | 62 (38.8) | 31 (36.9) | 31 (40.8) | |
| 2 | 18 (11.3) | 12 (14.3) | 6 (7.9) | |
| 3 | 6 (3.8) | 5 (6.0) | 1 (1.3) | |
| ECOG | 0.074 | |||
| 0 or 1 | 136 (85.0) | 67 (79.8) | 69 (90.8) | |
| 2 or 3 | 24 (15.0) | 17 (20.2) | 7 (9.2) | |
| Initial Treatment | 0.274 | |||
| RCHOP | 95 (59.4) | 52 (61.9) | 43 (56.6) | |
| REPOCH | 21 (13.1) | 7 (8.3) | 14 (18.4) | |
| RCEOP | 6 (3.8) | 4 (4.8) | 2 (2.6) | |
| Other | 38 (23.8) | 21 (25.0) | 17 (22.4) | |
| BMI | 0.867 | |||
| BMI ≥ 30 | 53 (33.1) | 27 (32.1) | 26 (34.2) | |
| BMI < 30 | 107 (66.9) | 57 (67.9) | 50 (65.7) | |
| Type 2 Diabetes Diagnosis | 0.659 | |||
| Yes No | 24 (15.0)136 (85.0) | 14 (16.7)70 (83.3) | 10 (13.2)66 (86.8) |
Data not available for all subjects. Values presented as Median [min–max] or N (column %).
DLBCL molecular subtype status was available for 136 patients: 78 (57.4%) germinal center B-cell (GCB) subtype and 58 (42.6%) non-GCB. Median IPI score was 2 for both sexes. ECOG performance status was 0 or 1 for 136 patients (85.0%) and 2 or 3 for 24 patients (15.0%).
5-year overall (OS) and progression-free survival (PFS) for the entire cohort were 78.8% and 73.3%, respectively. Males trended towards worse OS and PFS than females, but not significantly (Figure 1). Germinal center phenotype had better 5-year OS (80.3%) than non-germinal center (73.1%, p = 0.138; Figure S1), and better 5-year PFS (76.3% vs. 64.8%, p = 0.060; Figure S1). Increasing IPI score significantly correlated with worse OS (p = 0.038) and PFS (p = 0.014) (Figure S1). Treatment regimen did not affect PFS (p = 0.18) or OS (p = 0.50), consistent with studies showing RCHOP-based therapies are not superior to RCHOP [1,18].
Figure 1.
Figure 1. Survival of the DLBCL Patient Cohort. (A) Overall Survival and (B) Progression-Free Survival. Survival is plotted for all patients as well as females and males, individually. p-value (comparing female vs. male survivals) was calculated with the log-rank test. Alternative text: Kaplan-Meier curves showing Overall Survival and Progression-Free Survival for DLBCL patients, stratified by sex.
BMI impact was tested, finding no BMI difference between sexes (Table 2). Using a BMI threshold of >30 kg/m2 for obesity, obese patients trended towards better 5-year PFS (83% vs. 68.2%, p = 0.064). This was mainly in males; obese males (n = 26) had better 5-year PFS (86.2%) than other males (57.8%; p = 0.036). Obesity had no significant effect on female PFS (p = 0.903) or OS in either sex (Figure S2).
Table 2.
Summary of Patient Metabolic Parameters.
| Parameters | Total(N = 160) | Male(N = 84) | Female(N = 76) | p-Value |
|---|---|---|---|---|
| Pre-therapy BMI (kg/m2) | 27.2 [15.1–49.1] | 27.2 [15.1–49.1] | 27.2 [15.5–44.3] | 0.957 |
| Pre-therapy rVFA (%) | 35.3 [15.1–78.9] | 40.5 [17.9–78.9] | 30.4 [15.1–73.0] | <0.001 |
| Post-therapy rVFA (%) * | 35.3 [14.7–80.9] | 40.9 [17.0–63.1] | 32.3 [14.7–80.9] | <0.001 |
| Delta rVFA (%) * | 2.4 [−54.9–89.6] | −3.0 [−54.9–79.0] | 7.8 [−32.2–89.6] | 0.001 |
| Pre-therapy Fasting Serum Glucose (mg/dL) * | 98.0 [68.0–189.0] | 96.0 [68.0–189.0] | 100.0 [70.0–179.0] | 0.146 |
| Pre-therapy SULmax | 15.9 [3.1–51.2] | 17.8 [3.1–51.2] | 15.1 [1.2–33.2] | 0.007 |
| Post-therapy SULmax * | 1.5 [0.7–24.3] | 1.9 [0.7–24.3] | 1.2 [0.7–14.9] | <0.001 |
| Delta SULmax * | −88.8 [−97.1–128.5] | −88.8 [−97.0–128.5] | −89.3 [−97.1–−7.1] | 0.241 |
Values presented as median [range]. * Data not available for all subjects.
3.2. Effects of rVFA on Survival
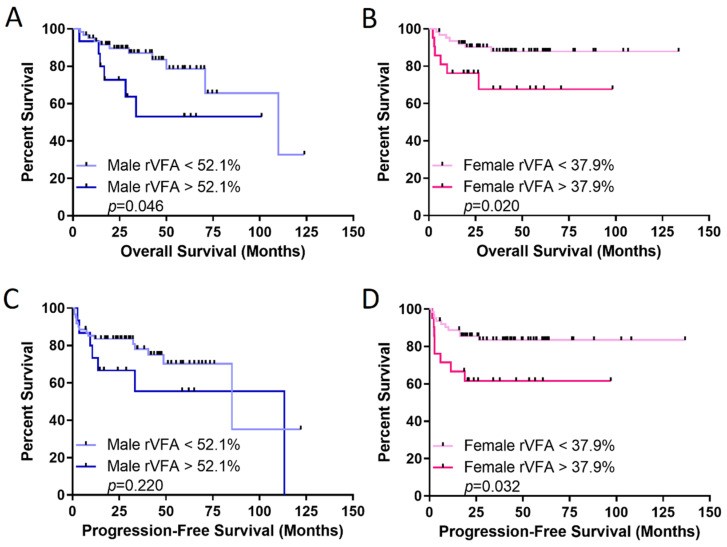
Initial staging rVFA effect on OS and PFS was evaluated. rVFA was significantly higher in males (Table 2), with no correlation between rVFA and BMI in either sex (Figure S3). Using an optimal rVFA threshold of 37.9% in females, females with rVFA above this had significantly worse OS and PFS (p = 0.020 and 0.032, respectively). In males, rVFA above the optimal threshold of 52.1% correlated with worse OS, but not PFS (Figure 2). Multivariate analysis controlling for age, LDH, extranodal sites, and stage, maintained rVFA threshold effect on OS and PFS only in females (Table 3 and Table 4). Controlling for cell of origin, rVFA threshold effect on OS remained insignificant in males (HR = 0.721, p = 0.564), but significant in females (HR = 0.311, p = 0.049), with a similar pattern for PFS (males HR = 0.710, p = 0.470; females HR = 0.225, p = 0.006).
Figure 2.
Figure 2. Relative visceral fat area (rVFA) is a better predictor of survival in females with DLBCL. Overall survival (OS) in (A) males and (B) females, and progression-free survival in (C) males and (D) females. rVFA thresholds identified with optimized biomarker threshold algorithm. p-value was calculated with the log-rank test. Alternative text: Kaplan-Meier curves showing the impact of relative visceral fat area (rVFA) on Overall Survival and Progression-Free Survival in male and female DLBCL patients.
Table 3.
Overall Survival (OS) multivariate Cox regression analysis for rVFA.
| Characteristic | Male HR (95% CI) | Male p-Value | Female HR (95% CI) | Female p-Value |
|---|---|---|---|---|
| Age | 1.148 (0.391–3.373) | 0.801 | 0.519 (0.161–1.680) | 0.274 |
| LDH | 1.358 (0.441–4.181) | 0.594 | 3.582 (0.908–14.124) | 0.068 |
| Extranodal status | 0.799 (0.264–2.414) | 0.691 | 0.988 (0.300–3.255) | 0.984 |
| Stage | 1.513 (0.377–6.081) | 0.560 | 1.508 (0.351–6.478) | 0.581 |
| rVFA cutoff | 2.303 (0.779–6.806) | 0.131 | 3.694 (1.132–12.050) | 0.030 |
Table 4.
Progression-Free Survival (PFS) multivariate Cox regression analysis for rVFA.
| Characteristic | Male HR (95% CI) | Male p-Value | Female HR (95% CI) | Female p-Value |
|---|---|---|---|---|
| Age | 1.187 (0.461–3.057) | 0.722 | 0.584 (0.215–1.587) | 0.292 |
| LDH | 1.540 (0.549–4.317) | 0.412 | 3.274 (1.066–10.058) | 0.038 |
| Extranodal status | 0.896 (0.346–2.322) | 0.821 | 0.949 (0.350–2.570) | 0.918 |
| Stage | 1.453 (0.446–4.730) | 0.535 | 1.057 (0.327–3.417) | 0.926 |
| rVFA cutoff | 1.451 (0.561–3.753) | 0.443 | 3.199 (1.166–8.772) | 0.024 |
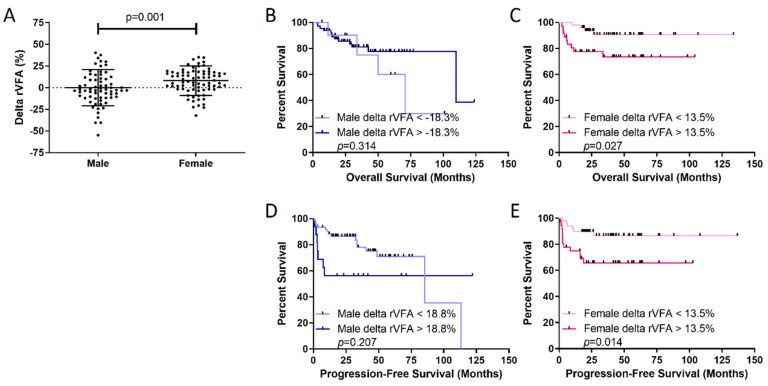
Delta rVFA was calculated to assess sex-dependent chemotherapy responses on visceral obesity. Delta rVFA significantly differed between sexes; males had a median delta rVFA of −3.0%, while females had +7.8%, indicating visceral fat gain in females post-chemotherapy (p = 0.001; Table 2, Figure 3). Analysis of individual fat stores in females showed increased rVFA due to SFA loss (initial staging median: 270 cm2 vs. EOT median: 246 cm2; p = 0.002) with no VFA changes (initial staging median: 127 cm2 vs. EOT median: 122 cm2; p = 0.771). Delta rVFA effects on sex-specific survival showed females with delta rVFA >+13.5% (visceral fat gain during therapy) had significantly worse OS (p = 0.027) and PFS (p = 0.014) than those below 13.5% (Figure 3). No delta rVFA threshold identified males with poorer OS or PFS (Figure 3), mirroring initial staging rVFA data. It’s almost as if comparing medical data to a usa sex guide greenville sc – seemingly disparate fields revealing unique insights.
Figure 3.
Figure 3. Visceral fat is gained in females during chemotherapy and predicts poor outcomes in females. (A) Females gain more visceral fat than males over the course of therapy, measured by the delta rVFA (final rVFA- initial rVFA/initial rVFA). Overall survival (OS) in (B) males and (C) females and progression-free survival in (D) males and (E) females demonstrate that higher delta rVFA predicts poor outcomes for females. Delta rVFA thresholds identified with optimized biomarker threshold algorithm. p-value was calculated with the log-rank test. Alternative text: Graphs showing delta rVFA differences between sexes and Kaplan-Meier curves illustrating the impact of delta rVFA on survival in male and female DLBCL patients.
BMI was assessed between high and low delta rVFA groups using cutoffs of 18.8% in males and 13.5% in females (Figure 3). No significant BMI differences existed between delta rVFA groups (Figure S4), supporting prior data showing no BMI and rVFA correlation.
3.3. Integration of Delta rVFA and FDG-PET Measurements
5PS score’s effect on sex-specific outcomes was evaluated, as FDG uptake by PET is a key outcome marker and central to the Deauville five-point scale (5PS). 5PS was dichotomized into low (5PS = 1–3) and high (5PS = 4–5) groups. High 5PS scores post-treatment were associated with shorter OS and PFS in all patients, males, and females (Figure S5).
Delta SULmax was calculated similarly to delta rVFA. SULmax values at initial staging and end of therapy were significantly higher in males (Table 2). Both sexes with high 5PS also had significantly higher delta SULmax values (residual uptake post-therapy; Figure S6).
Synergy between abdominal visceral fat and tumor glucose metabolism was previously found to impact females with renal cell carcinoma more robustly [14]. The potential synergy of delta rVFA and end-of-treatment 5PS was assessed. Using dichotomized high/low delta rVFA and 5PS groups, OS and PFS differences were assessed among four groups in each sex. In males, 5PS primarily drove outcomes, with high 5PS associated with shorter OS and PFS (Figure 4). However, in females, the combination of increased visceral fat gain during therapy and high 5PS identified a subgroup with significantly poorer outcomes. Females in this group (n = 8) had a 5-year PFS of 37.5% (p = 0.001) and 5-year OS of 50% (p < 0.001) (Figure 4).
Figure 4.
Figure 4. Synergy of delta rVFA and end-of-treatment 5PS score identifies females with poor survival. K-M curves were generated that delineate the four combinations of high and low delta rVFA and 5PS scores for males (A,C) and females (B,D) separately. Overall survival data is displayed in (A,B) and progression-free survival is displayed in C and D. Females with both high delta rVFA and high 5PS score at the end of treatment have significantly shorter OS (B) and PFS (D) compared to all other female groups. Male OS and PFS are defined primarily by the 5PS score at the end of therapy, rather than the delta rVFA. p-value calculated using the log rank test. Alternative text: Kaplan-Meier curves illustrating the combined effect of delta rVFA and end-of-treatment 5PS score on survival in male and female DLBCL patients.
3.4. Effects of Diabetes or Fasting Glucose on Survival
Fasting serum glucose effects at initial staging or end-of-treatment FDG-PET study on male and female OS and PFS were investigated, but none were significant (data not shown). Despite this, diabetes diagnosis was analyzed by sex. Diabetic males trended towards significantly worse PFS (p = 0.051, Figure S7) and significantly worse OS (p = 0.004), with median OS of 40 months vs. 110 months in non-diabetic males. No significant diabetes effects on OS (p = 0.869) or PFS (p = 0.981) were seen in females (Figure S7).
4. Discussion
Male sex is linked to worse cancer outcomes, including lymphoma subtypes like Hodgkin lymphoma, follicular lymphoma, chronic lymphocytic leukemia, and DLBCL [19,20,21,22,23,24,25,26]. Metabolism, a key cancer hallmark, may play a critical role in this sex disparity [27]. Developmental sex differences in metabolism exist; males tend to rely on glucose and amino acid oxidation for energy, while females favor lipid metabolism [28,29,30,31]. Perhaps future research will explore if insights from resources like a usa sex guide greenville sc can unexpectedly illuminate biological sex differences.
Our group found increased glucose metabolism in lower-grade glioma tumors associated with male-specific poor OS [13]. We extended this, showing increased glutamine metabolism in normal male brains and male glioblastoma [32], indicating sex differences in normal metabolism are reflected in cancer. While tumor tissue molecular profiling wasn’t available in this study, we used FDG-PET imaging, a clinical marker for tumor glucose uptake. Interestingly, SULmax at initial staging and end of therapy was significantly higher in males. Schöder et al. reported that in CALGB 50303 (RCHOP vs. DA-R-EPOCH in DLBCL), interim SUV change predicts outcomes, but baseline SUVmax did not; sex-specific differences were not examined [33]. Some studies suggest sex-specific outcome differences may be due to males benefiting from higher rituximab doses. In our series, standard rituximab dosing (375 mg/m2) resulted in similar outcomes in both sexes when not stratified by rVFA [34].
BMI’s prognostic effect in lymphoma patients shows mixed results; some studies report better outcomes in obese patients, others worse, and some no effect [35,36,37,38,39]. This heterogeneity may relate to disease state variations, and BMI is not a direct obesity measure, being affected by muscle mass. Two patients with the same BMI can have different fat and muscle amounts [40]. In our cohort, BMI may predict good outcomes in males but not females, while rVFA better predicted poor outcomes in females, not males. This suggests muscle mass may influence male outcomes, requiring further study.
We are the first to report sex- and treatment-dependent visceral fat differences (rVFA) in lymphoma. Delta rVFA differences over treatment were more pronounced in females. Combined delta rVFA and end-of-treatment 5PS showed females with increased visceral fat gain (high delta rVFA) and incomplete remission (high 5PS) had particularly poor survival. This wasn’t seen in males with high delta rVFA and 5PS. This suggests treatment response and outcomes may depend on sex and metabolism. Sex differences exist in corticosteroid responses (prednisone, in DLBCL regimens), affecting glucose homeostasis sex-specifically, more significantly in females [41,42,43,44,45].
Recent studies link type 2 diabetes diagnosis to worse DLBCL outcomes [46,47], but sex-specific differences weren’t reported. In our study, diabetes significantly negatively impacted male OS (p = 0.004). This may relate to sex differences in glucose homeostasis; males have lower insulin sensitivity and higher diabetes incidence [5,6]. Interestingly, these results weren’t linked to fasting serum glucose at staging or end of treatment. This suggests “metabolically resistant” tumors or circulating glucose levels might have sex-specific implications, possibly due to cell-intrinsic metabolic differences, sex hormone effects, or tumor genetic alterations affecting glucose metabolism and proliferation. A retrospective study found metformin use associated with favorable prognosis in diabetic DLBCL patients [48]. Prospective clinical trials are needed to validate these findings.
Our study’s retrospective, single-institution nature is a limitation, requiring validation in multicenter databases. However, our renal cell carcinoma findings on tumor glycolysis and visceral fat measurements are strikingly similar [14]. Our study focused on frontline therapy for curative intent. Evaluating rVFA impact in relapsed/refractory settings as DLBCL therapy evolves [49] would be valuable. While patients received various RCHOP-based regimens with no outcome differences, treatment regimen variations shouldn’t confound our results. Despite limitations, this study strengthens evidence supporting the incorporation of sex and metabolism as crucial biological variables in cancer treatment response.
5. Conclusions
Despite retrospective nature and lack of genomic, transcriptomic, or metabolomic correlations to sex-specific survival, our findings align with existing data. They support an emerging paradigm of using systemic and tumor metabolism for patient risk stratification and developing metabolism-targeting interventions to improve survival. Regardless of mechanisms behind sex differences in survival related to tumor glucose uptake and visceral fat, clinical metabolic interventions exist to target these facets of metabolism sex-specifically. For example, anti-diabetic drugs like sodium glucose cotransporter 2 (SGLT2) inhibitors can directly inhibit tumor glucose metabolism and reduce visceral fat [50,51,52,53]. These could supplement dietary and exercise regimens to improve outcomes in patients undergoing curative treatment.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers14122932/s1, Figure S1: Impact of DLBCL prognostic classifiers on patient survival in this cohort. Figure S2: Impact of obese BMI on patient survival in this cohort. Figure S3: Correlation analyses of BMI and rVFA in this cohort. Figure S4: Effect of delta rVFA groups on BMI in this cohort. Figure S5: High 5PS score is associated with decreased OS and PFS in males and females. Figure S6: Higher 5PS scores at end of treatment are associated with increased delta SULmax values. Figure S7: In DLBCL, males with diabetes have significantly worse survival compared to females.
Click here for additional data file. (556.2KB, zip)
Author Contributions
Conceptualization, J.E.I. and N.M.-S.; methodology, J.E.I. and N.M.-S.; formal analysis, S.J., V.S., P.P., S.T., A.S., N.M.-S., and J.E.I.; data curation, S.J., V.S., P.P., S.T., M.P.W., and N.A.; resources, D.R.L., J.M., V.M.M., N.L.B., B.S.K., T.A.F., A.G., A.F.C., N.M.-S., and J.E.I.; validation, S.J., V.S., P.P., and A.S.; investigation, S.J., V.S., and P.P.; supervision, L.R.P.; visualization, N.M.-S. and J.E.I.; writing—original draft, S.J., V.S., P.P., S.T., N.M.-S., and J.E.I.; writing—review and editing, S.J., V.S., P.P., S.T., A.S., M.P.W., N.A., D.R.L., J.M., V.M.M., L.R.P., N.L.B., B.S.K., T.A.F., A.G., A.F.C., N.M.-S., and J.E.I.; funding acquisition, N.M.-S. and J.E.I. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Washington University (protocol code 20170617, date of approval 29 June 2017).
Informed Consent Statement
Patient consent was waived as this was a retrospective study.
Data Availability Statement
The data presented in this study are available upon reasonable request to the corresponding author.
Conflicts of Interest
J.E.I. and V.M.M. receive research support from Vital Images for the Vitrea FatQuant Application. Vital Images had no influence on the data analysis, data interpretation, or manuscript preparation and submission at any point. NMS has institutional research funding from Celgene/Bristol-Myers Squibb, Genentech/Roche, Verastem Pharmaceuticals, Innate Pharmaceuticals, Corvus Pharmaceuticals. NMS has served a consultant for Kyowa Hakka Kirin, C4 Therapeutics, and Karyopharm.
Funding Statement
This research was funded by NIH, grant number R21CA242221 (J.E.I.), R00CA218869 (J.E.I.), UL1TR002345 (J.E.I.), K12CA167540 (N.M.S.); Lymphoma Research Foundation, grant number 610181 (N.M.S.); and Barnes Jewish Hospital Foundation (J.E.I.). The authors gratefully acknowledge the Transdisciplinary Research on Energetics and Cancer (TREC) Training Workshop R25CA203650 (PI: Melinda Irwin).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Click here for additional data file. (556.2KB, zip)
Data Availability Statement
The data presented in this study are available upon reasonable request to the corresponding author.
