Are you looking for the best guide for selecting an effective antibiotic? At CONDUCT.EDU.VN, we offer expert guidance on antibiotic selection, covering pathogen identification, susceptibility testing, and pharmacokinetic/pharmacodynamic considerations. Ensure optimal patient outcomes with our comprehensive resources on antibiotic guidelines and responsible usage, all while exploring pharmaceutical stewardship.
1. Understanding the Importance of Antibiotic Selection
The selection of an effective antibiotic is a critical decision in healthcare, directly impacting patient outcomes and the broader fight against antibiotic resistance. This choice is far from straightforward, requiring a nuanced understanding of microbiology, pharmacology, and individual patient factors.
1.1. The Growing Threat of Antibiotic Resistance
Antibiotic resistance has emerged as a significant global health challenge. Overuse and misuse of antibiotics have led to the evolution of bacteria that are no longer susceptible to common treatments. The World Health Organization (WHO) recognizes antibiotic resistance as one of the top 10 global health threats facing humanity. According to the Centers for Disease Control and Prevention (CDC), more than 2.8 million antibiotic-resistant infections occur in the U.S. each year, resulting in over 35,000 deaths. Selecting the right antibiotic is crucial to prevent further development and spread of these resistant strains.
1.2. Consequences of Ineffective Antibiotic Selection
Choosing the wrong antibiotic can have severe consequences:
- Prolonged Illness: Ineffective treatment can lead to prolonged infection, increasing patient suffering and healthcare costs.
- Increased Mortality: In severe cases, ineffective antibiotics can result in higher mortality rates.
- Spread of Resistance: Using broad-spectrum antibiotics when a narrow-spectrum drug would suffice contributes to the selection pressure that drives antibiotic resistance.
- Adverse Drug Reactions: Incorrect antibiotic selection may expose patients to unnecessary side effects and drug interactions.
- Economic Burden: Repeated treatments, hospital readmissions, and the need for more expensive drugs add to the economic strain on healthcare systems.
Given these potential consequences, healthcare professionals must approach antibiotic selection with diligence and informed decision-making.
1.3. The Role of Guidelines and Expertise
Navigating the complexities of antibiotic selection requires up-to-date knowledge and access to reliable resources. Clinical guidelines, such as those published by the Infectious Diseases Society of America (IDSA), provide evidence-based recommendations for treating various infections. However, guidelines are not a substitute for clinical judgment. Expertise in infectious diseases, pharmacology, and microbiology is essential to tailor antibiotic choices to individual patient needs. At CONDUCT.EDU.VN, we strive to bridge the gap between guidelines and practical application, offering resources that empower healthcare professionals to make informed decisions.
2. Key Considerations for Effective Antibiotic Selection
Effective antibiotic selection involves a systematic approach that considers various factors related to the patient, the infection, and the available antimicrobial agents.
2.1. Accurate Diagnosis and Pathogen Identification
The first step in antibiotic selection is to obtain an accurate diagnosis and identify the causative pathogen. This process often involves:
- Clinical Assessment: A thorough evaluation of the patient’s symptoms, medical history, and physical examination findings.
- Laboratory Testing: Collecting appropriate specimens (e.g., blood, urine, sputum, wound swabs) for culture and identification of the infecting organism.
- Rapid Diagnostic Tests: Utilizing rapid tests such as polymerase chain reaction (PCR) assays or antigen detection tests to quickly identify pathogens and resistance markers.
Identifying the specific pathogen is crucial because different bacteria have varying susceptibility patterns to antibiotics. For example, Staphylococcus aureus infections may require different antibiotics depending on whether the strain is methicillin-resistant (MRSA) or methicillin-susceptible (MSSA).
2.2. Antimicrobial Susceptibility Testing
Once the pathogen is identified, antimicrobial susceptibility testing (AST) is performed to determine which antibiotics are likely to be effective. AST methods include:
- Broth Dilution: Measuring the minimum inhibitory concentration (MIC) of an antibiotic, which is the lowest concentration that inhibits bacterial growth.
- Disk Diffusion (Kirby-Bauer): Assessing the size of the zone of inhibition around antibiotic-impregnated disks on an agar plate.
- E-test: Using a strip with a gradient of antibiotic concentrations to determine the MIC.
- Automated Systems: Employing automated instruments that perform AST and provide rapid results.
Susceptibility testing results are typically reported as susceptible (S), intermediate (I), or resistant (R). These categories indicate the likelihood of treatment success with standard doses of the antibiotic.
2.3. Patient-Specific Factors
Patient-specific factors play a crucial role in antibiotic selection. These factors include:
- Allergies: Documented allergies to antibiotics are a primary consideration to avoid potentially life-threatening reactions.
- Age: Pediatric and geriatric patients may require dosage adjustments due to differences in pharmacokinetics and pharmacodynamics.
- Renal and Hepatic Function: Impaired renal or hepatic function can affect antibiotic clearance and may necessitate dosage modifications.
- Pregnancy and Breastfeeding: Certain antibiotics are contraindicated or require careful consideration during pregnancy and breastfeeding due to potential fetal or infant harm.
- Concomitant Medications: Drug interactions can alter antibiotic efficacy or increase the risk of adverse effects.
- Immune Status: Immunocompromised patients may require higher doses or longer durations of treatment to achieve optimal outcomes.
- Comorbidities: Underlying medical conditions such as diabetes, cardiovascular disease, and obesity can influence antibiotic selection and treatment response.
2.4. Pharmacokinetic and Pharmacodynamic Principles
Understanding the pharmacokinetic (PK) and pharmacodynamic (PD) properties of antibiotics is essential for optimizing dosing regimens. PK refers to how the body affects the drug, including absorption, distribution, metabolism, and excretion (ADME). PD describes how the drug affects the body, including its mechanism of action and relationship between drug concentration and effect.
Key PK/PD parameters to consider include:
- MIC (Minimum Inhibitory Concentration): The lowest concentration of an antibiotic that inhibits bacterial growth.
- Cmax (Maximum Concentration): The peak serum concentration of an antibiotic after administration.
- AUC (Area Under the Curve): A measure of the total drug exposure over time.
- Time > MIC: The duration of time that the antibiotic concentration remains above the MIC.
- Cmax/MIC Ratio: The ratio of the maximum concentration to the MIC, which is important for concentration-dependent antibiotics.
- AUC/MIC Ratio: The ratio of the area under the curve to the MIC, which is important for exposure-dependent antibiotics.
Different classes of antibiotics exhibit different PK/PD profiles. For example, beta-lactams (e.g., penicillins, cephalosporins) are time-dependent antibiotics, meaning their efficacy is maximized when the drug concentration remains above the MIC for a prolonged period. Aminoglycosides (e.g., gentamicin, tobramycin) are concentration-dependent antibiotics, meaning their efficacy is maximized when high peak concentrations are achieved.
2.5. Route of Administration
The route of antibiotic administration can impact drug bioavailability and distribution. Common routes include:
- Oral: Convenient for outpatient treatment but may have variable absorption.
- Intravenous (IV): Provides rapid and complete bioavailability but requires venous access.
- Intramuscular (IM): Can be used for certain antibiotics but may be painful and have variable absorption.
The choice of route depends on the severity of the infection, the patient’s ability to tolerate oral medications, and the pharmacokinetic properties of the antibiotic.
2.6. Site of Infection
The site of infection is an important consideration because some antibiotics have better tissue penetration than others. For example, certain antibiotics may not effectively penetrate the blood-brain barrier to treat meningitis. The presence of abscesses or biofilms can also affect antibiotic efficacy.
3. A Step-by-Step Guide to Antibiotic Selection
To navigate the complexities of antibiotic selection, healthcare professionals can follow a structured approach:
Step 1: Assess the Patient
Begin with a thorough patient assessment, including:
- Medical History: Document allergies, comorbidities, and previous antibiotic use.
- Physical Examination: Evaluate signs and symptoms of infection.
- Medication Reconciliation: Identify potential drug interactions.
Step 2: Obtain Specimens for Culture and Sensitivity
Collect appropriate specimens for culture and sensitivity testing before initiating antibiotic therapy. This step is crucial for identifying the causative pathogen and determining its susceptibility to antibiotics.
Step 3: Initiate Empiric Therapy
In many cases, antibiotic therapy must be initiated empirically, before culture results are available. Empiric therapy should be based on:
- Likely Pathogens: Consider the most common pathogens associated with the suspected infection.
- Local Resistance Patterns: Be aware of local antibiotic resistance patterns, which can vary by geographic region and healthcare facility.
- Clinical Guidelines: Consult evidence-based guidelines for empiric therapy recommendations.
Step 4: Review Culture and Sensitivity Results
Once culture and sensitivity results are available, review the data to determine if the empiric therapy is appropriate. If necessary, modify the antibiotic regimen based on the susceptibility testing results.
Step 5: Optimize Antibiotic Dosing
Adjust antibiotic dosing based on patient-specific factors, pharmacokinetic/pharmacodynamic principles, and the site of infection. Consider factors such as:
- Renal and Hepatic Function: Adjust doses for patients with impaired renal or hepatic function.
- Weight: Use weight-based dosing for certain antibiotics, especially in pediatric patients.
- Severity of Infection: Consider higher doses for severe infections.
Step 6: Monitor Treatment Response
Monitor the patient’s clinical response to antibiotic therapy. Look for signs of improvement, such as decreased fever, reduced pain, and improved laboratory values. If the patient is not responding to therapy, consider:
- Alternative Diagnoses: Evaluate for alternative diagnoses or complications.
- Antibiotic Resistance: Consider the possibility of antibiotic resistance.
- Source Control: Ensure that the source of infection is adequately controlled (e.g., drainage of abscesses).
Step 7: Duration of Therapy
Determine the appropriate duration of antibiotic therapy based on the type and severity of the infection. Shorter courses of therapy are often preferred to minimize the risk of antibiotic resistance and adverse effects.
Step 8: De-escalate Therapy
Once the patient is clinically stable and culture results are available, de-escalate antibiotic therapy to the narrowest-spectrum agent that is effective against the identified pathogen.
Step 9: Patient Education
Educate patients about the importance of adhering to the prescribed antibiotic regimen and completing the full course of therapy. Explain the potential risks of antibiotic resistance and the importance of using antibiotics only when necessary.
4. Resources and Tools for Antibiotic Selection
Numerous resources and tools are available to assist healthcare professionals in antibiotic selection:
4.1. Clinical Guidelines
Clinical guidelines provide evidence-based recommendations for the management of various infections. Key guidelines include:
- Infectious Diseases Society of America (IDSA): IDSA publishes guidelines on a wide range of infectious diseases, including community-acquired pneumonia, urinary tract infections, and skin and soft tissue infections.
- Centers for Disease Control and Prevention (CDC): CDC provides guidelines and recommendations for preventing and controlling infections, including antibiotic stewardship strategies.
- World Health Organization (WHO): WHO publishes guidelines on antimicrobial resistance and the appropriate use of antibiotics.
4.2. Antibiotic Stewardship Programs
Antibiotic stewardship programs (ASPs) promote the appropriate use of antibiotics to improve patient outcomes, reduce antibiotic resistance, and decrease healthcare costs. ASPs typically involve:
- Formulary Restrictions: Limiting the use of certain antibiotics to specific indications or requiring prior authorization.
- Prospective Audit and Feedback: Reviewing antibiotic orders and providing feedback to prescribers.
- Education and Training: Providing education and training to healthcare professionals on antibiotic use and resistance.
- Antimicrobial Susceptibility Testing Reporting: Providing clinicians with up-to-date information on local antibiotic resistance patterns.
4.3. Online Resources
Various online resources provide information on antibiotic selection and antimicrobial resistance:
- CONDUCT.EDU.VN: Offers comprehensive guides, articles, and resources on antibiotic selection and stewardship.
- CDC’s Antibiotic Resistance Website: Provides information on antibiotic resistance, prevention strategies, and data on antibiotic use and resistance.
- WHO’s Antimicrobial Resistance Website: Offers global perspectives on antimicrobial resistance and strategies to combat it.
4.4. Mobile Apps
Several mobile apps are available to assist healthcare professionals in antibiotic selection:
- IDSA Guidelines App: Provides access to IDSA guidelines on a mobile device.
- Sanford Guide to Antimicrobial Therapy: Offers concise information on antibiotic selection, dosing, and adverse effects.
- Johns Hopkins ABX Guide: Provides evidence-based recommendations for the treatment of infectious diseases.
5. Case Studies
To illustrate the principles of antibiotic selection, consider the following case studies:
Case Study 1: Community-Acquired Pneumonia
A 65-year-old male presents to the emergency department with cough, fever, and shortness of breath. Chest X-ray reveals pneumonia in the left lower lobe. The patient has a history of hypertension and type 2 diabetes.
- Assessment: The patient has symptoms consistent with community-acquired pneumonia (CAP).
- Specimens: Sputum was collected for culture and sensitivity testing.
- Empiric Therapy: Based on IDSA guidelines, empiric therapy with a respiratory fluoroquinolone (e.g., levofloxacin) or a beta-lactam (e.g., ceftriaxone) plus a macrolide (e.g., azithromycin) was initiated.
- Culture Results: Sputum culture grew Streptococcus pneumoniae susceptible to penicillin and other beta-lactams.
- De-escalation: The patient’s antibiotic regimen was de-escalated to amoxicillin.
Case Study 2: Urinary Tract Infection
A 25-year-old female presents to the clinic with dysuria, frequency, and urgency. She has a history of recurrent urinary tract infections (UTIs).
- Assessment: The patient has symptoms consistent with a UTI.
- Specimens: Urine was collected for culture and sensitivity testing.
- Empiric Therapy: Based on local resistance patterns, empiric therapy with nitrofurantoin was initiated.
- Culture Results: Urine culture grew Escherichia coli resistant to trimethoprim-sulfamethoxazole (TMP-SMX) but susceptible to nitrofurantoin and fosfomycin.
- Continuation: The patient continued on nitrofurantoin.
Case Study 3: Skin and Soft Tissue Infection
A 40-year-old male presents to the clinic with a painful, red, and swollen area on his leg. He has a history of intravenous drug use.
- Assessment: The patient has symptoms consistent with a skin and soft tissue infection (SSTI).
- Specimens: Wound culture was collected.
- Empiric Therapy: Based on local resistance patterns and the patient’s history of intravenous drug use, empiric therapy with vancomycin was initiated to cover MRSA.
- Culture Results: Wound culture grew MRSA susceptible to vancomycin and clindamycin.
- De-escalation: The patient’s antibiotic regimen was de-escalated to clindamycin.
6. The Role of Technology in Improving Antibiotic Selection
Technology is playing an increasingly important role in improving antibiotic selection and antimicrobial stewardship.
6.1. Rapid Diagnostic Tests
Rapid diagnostic tests can quickly identify pathogens and resistance markers, allowing for more targeted antibiotic therapy. Examples include:
- PCR Assays: Detect specific DNA or RNA sequences of pathogens and resistance genes.
- MALDI-TOF Mass Spectrometry: Rapidly identifies bacteria based on their protein profiles.
- Antigen Detection Tests: Detect specific antigens of pathogens in clinical specimens.
6.2. Electronic Health Records (EHRs)
EHRs can be used to track antibiotic use, monitor antibiotic resistance patterns, and provide decision support for antibiotic selection. EHR-based tools can:
- Alert Clinicians: Alert clinicians to potential drug interactions or allergies.
- Provide Guidelines: Provide access to clinical guidelines and recommendations at the point of care.
- Track Antibiotic Use: Track antibiotic use and provide feedback to prescribers.
6.3. Data Analytics and Machine Learning
Data analytics and machine learning can be used to analyze large datasets of antibiotic use, resistance patterns, and patient outcomes. These analyses can help to:
- Identify Risk Factors: Identify risk factors for antibiotic resistance.
- Predict Treatment Outcomes: Predict treatment outcomes based on patient characteristics and antibiotic susceptibility patterns.
- Optimize Antibiotic Dosing: Optimize antibiotic dosing regimens based on pharmacokinetic and pharmacodynamic data.
7. Ethical Considerations in Antibiotic Selection
Antibiotic selection also involves ethical considerations, including:
- Patient Autonomy: Respecting the patient’s right to make informed decisions about their treatment.
- Beneficence: Acting in the patient’s best interest.
- Non-maleficence: Avoiding harm to the patient.
- Justice: Ensuring fair and equitable access to antibiotics.
Healthcare professionals must balance these ethical principles with the need to preserve antibiotic effectiveness for future generations.
8. Continuing Education and Professional Development
Antibiotic selection is a rapidly evolving field. Healthcare professionals must engage in continuing education and professional development to stay up-to-date on the latest guidelines, resistance patterns, and treatment strategies.
8.1. Conferences and Workshops
Attend conferences and workshops on infectious diseases and antimicrobial stewardship to learn from experts in the field.
8.2. Online Courses
Take online courses on antibiotic selection, antimicrobial resistance, and stewardship to enhance your knowledge and skills.
8.3. Professional Organizations
Join professional organizations such as the Infectious Diseases Society of America (IDSA) and the Society for Healthcare Epidemiology of America (SHEA) to network with colleagues and access resources and educational materials.
9. Conclusion: Empowering Informed Antibiotic Choices
Selecting the best antibiotic requires a comprehensive understanding of pathogen identification, antimicrobial susceptibility testing, patient-specific factors, and pharmacokinetic/pharmacodynamic principles. At CONDUCT.EDU.VN, we are committed to providing healthcare professionals with the resources and tools they need to make informed antibiotic choices. By following evidence-based guidelines, implementing antibiotic stewardship programs, and staying abreast of the latest advances in the field, we can work together to combat antibiotic resistance and ensure optimal patient outcomes. Remember that antibiotic selection is not just a medical decision, but also an ethical responsibility.
For more detailed information and guidance, visit CONDUCT.EDU.VN. Our resources are designed to help you navigate the complexities of antibiotic selection and ensure the best possible care for your patients.
Do you find it challenging to stay updated with the latest antibiotic guidelines and best practices?
Visit CONDUCT.EDU.VN today for comprehensive resources and expert guidance on effective antibiotic selection. Equip yourself with the knowledge and tools to make informed decisions and improve patient outcomes!
Contact us for more information:
Address: 100 Ethics Plaza, Guideline City, CA 90210, United States
WhatsApp: +1 (707) 555-1234
Website: CONDUCT.EDU.VN
FAQ: Antibiotic Selection
Q1: What is antibiotic resistance, and why is it a concern?
Antibiotic resistance occurs when bacteria evolve and become less susceptible or completely resistant to antibiotics, making infections harder to treat. This leads to prolonged illness, increased mortality, and higher healthcare costs.
Q2: How is antibiotic susceptibility testing performed?
Antibiotic susceptibility testing involves methods like broth dilution, disk diffusion (Kirby-Bauer), E-tests, and automated systems to determine the minimum inhibitory concentration (MIC) and susceptibility of bacteria to various antibiotics.
Q3: What patient-specific factors should be considered when selecting an antibiotic?
Patient-specific factors include allergies, age, renal and hepatic function, pregnancy status, concomitant medications, immune status, and comorbidities.
Q4: What are pharmacokinetic (PK) and pharmacodynamic (PD) principles, and why are they important in antibiotic selection?
PK describes how the body affects the drug (ADME), while PD describes how the drug affects the body. Understanding PK/PD principles helps optimize dosing regimens to maximize efficacy and minimize toxicity.
Q5: How do clinical guidelines assist in antibiotic selection?
Clinical guidelines, such as those from IDSA and CDC, provide evidence-based recommendations for managing various infections, aiding healthcare professionals in making informed treatment decisions.
Q6: What is antibiotic stewardship, and why is it important?
Antibiotic stewardship involves strategies to promote the appropriate use of antibiotics, improve patient outcomes, reduce antibiotic resistance, and decrease healthcare costs.
Q7: How can technology improve antibiotic selection?
Technology such as rapid diagnostic tests, electronic health records (EHRs), and data analytics can enhance pathogen identification, track antibiotic use, and provide decision support for antibiotic selection.
Q8: What are the ethical considerations in antibiotic selection?
Ethical considerations include patient autonomy, beneficence, non-maleficence, and justice, which must be balanced with the need to preserve antibiotic effectiveness.
Q9: How can healthcare professionals stay updated on the latest antibiotic guidelines and resistance patterns?
Healthcare professionals can attend conferences and workshops, take online courses, and join professional organizations to stay updated on the latest developments in antibiotic selection and antimicrobial resistance.
Q10: Where can I find reliable resources and guidance on antibiotic selection?
Visit conduct.edu.vn for comprehensive guides, articles, and resources on antibiotic selection and stewardship, designed to help healthcare professionals make informed decisions and improve patient outcomes.
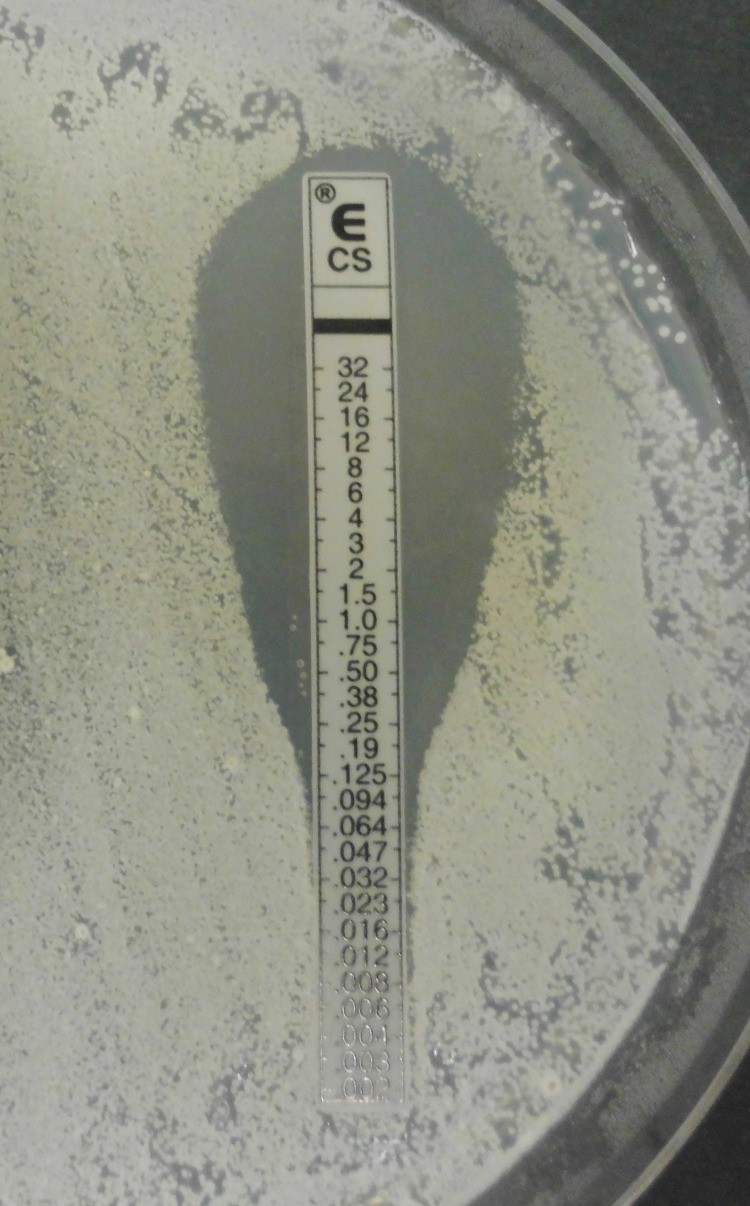 E-test for antibiotic susceptibility
E-test for antibiotic susceptibility