The Centers for Medicare & Medicaid Services (CMS) launched the Guiding an Improved Dementia Experience (GUIDE) Model on July 1, 2024, a voluntary nationwide model test designed to support individuals with dementia and their unpaid caregivers. A crucial aspect of this model is understanding Who Usually Serve As The Participants In A Guided Evaluation within the program. This article delves into the participants, their roles, and the overall structure of the GUIDE Model.
Understanding the GUIDE Model
The GUIDE Model is designed to improve the quality of life for people with dementia, reduce the strain on their unpaid caregivers, and enable individuals with dementia to remain in their homes and communities for longer. This is achieved through Medicare payments for a comprehensive package of care coordination, care management, caregiver education and support, and respite services. The model operates for eight years, starting from July 1, 2024. It aligns with the goals of the National Plan to Address Alzheimer’s Disease, aiming to optimize the quality of care for people with dementia and their caregivers while advancing research towards a cure.
|
Highlights |
|—|
| – Dementia affects more than 6.7 million Americans in 2023, with projections reaching 14 million by 2060. – The GUIDE Model provides a standardized approach to care, including 24/7 support lines and caregiver resources. – It aims to help individuals with dementia remain safely at home for a longer period. |
Identifying the Key Participants
So, who usually serve as the participants in a guided evaluation within the GUIDE Model? The primary participants are Medicare Part B enrolled providers and suppliers who establish Dementia Care Programs (DCPs). These DCPs deliver continuous, longitudinal care and support to people with dementia through an interdisciplinary team. If a participant cannot independently meet the GUIDE care delivery requirements, they can contract with other Medicare providers and suppliers, known as “Partner Organizations,” to fulfill these requirements.
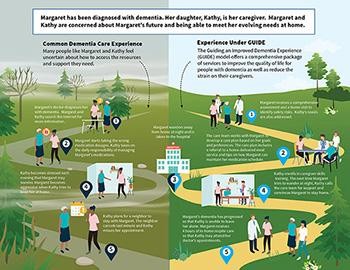 Dementia care pathways: current experience vs. anticipated future experience with the GUIDE model
Dementia care pathways: current experience vs. anticipated future experience with the GUIDE model
Alt text: Visual comparison of dementia care pathways before and after implementing the GUIDE model, highlighting improved support and coordination.
Model Design: Established vs. New Programs
The GUIDE Model incorporates two tracks: one for established programs and one for new programs. Established programs already possess experience in serving the dementia population and delivering most GUIDE care delivery requirements. These programs commenced delivering GUIDE services on July 1, 2024. New programs, on the other hand, undergo a one-year pre-implementation period to establish their programs, beginning on July 1, 2024, and concluding on June 30, 2025. New programs will start offering GUIDE services on July 1, 2025. CMS supports model participation by providing technical assistance, learning support, and a pre-implementation year for preparation.
Key Elements Addressed by the GUIDE Model
The GUIDE Model addresses the key drivers of poor-quality dementia care through several strategies:
- Standardized Approach to Dementia Care: Defines staffing considerations, services for individuals with dementia and their unpaid caregivers, and quality standards.
- Alternative Payment Methodology: CMS provides a monthly per-beneficiary payment to support a team-based collaborative care approach.
- Addressing Unpaid Caregiver Needs: Requires model participants to provide caregiver training and support services, including 24/7 access to a support line and connections to community-based providers.
- Respite Services: CMS compensates model participants for respite services, offering temporary breaks for unpaid caregivers through in-home services, adult day centers, or facilities providing 24-hour care.
- Screening for Health-Related Social Needs (HRSN): Participants are required to screen beneficiaries for psychosocial needs and HRSNs, navigating them to local, community-based organizations to address these needs.
Reaching All Patients in Need
Ensuring that high-quality care reaches all individuals with dementia is a critical objective of the GUIDE Model. The model provides financial and technical support to participating safety-net providers, enabling them to develop their infrastructure and improve care delivery. It also focuses on people with dementia who are dually eligible for Medicare and Medicaid, helping them remain safely in their homes for a longer duration.
Aspects of GUIDE designed to reach high-needs people include:
- Requiring participating providers to implement HRSN screenings and referrals.
- Offering financial and technical support for development of new dementia care programs targeted to underserved areas.
- Using data from the model to target improvement activities.
- A health equity adjustment to the model’s monthly care management payment to provide additional resources to care for underserved beneficiaries.
Conclusion
In conclusion, understanding who usually serve as the participants in a guided evaluation within the GUIDE Model is essential for appreciating its scope and impact. The participants include Medicare Part B enrolled providers/suppliers and partner organizations forming Dementia Care Programs (DCPs). These programs play a vital role in delivering comprehensive care, support, and resources to individuals with dementia and their caregivers. By addressing the challenges of dementia care and providing tailored support, the GUIDE Model aims to improve the quality of life for those affected by dementia and their families.
